B. J. Flink1,2, Y. Liu3,4, R. Rochat3, D. A. Kooby1,4, J. Lipscomb3,4, T. W. Gillespie1,4 1Emory University School Of Medicine,Surgery,Atlanta, GA, USA 2VA Atlanta Health System,Surgery,Atlanta, GA, USA 3Emory University Rollins School Of Public Health,Atlanta, GA, USA 4Winship Cancer Institue,Atlanta, GA, USA
Introduction: Pancreatic adenocarcinoma (PA) is a lethal cancer that newly affects over 41,000 Americans annually. Prior evidence demonstrates treatment and survival disparities between black and white patients. Our study examines receipt of surgery and overall survival by race, using novel data from a large population cancer database.
Methods: Using the National Cancer Data Base Participant User Files from 2003 to 2011, we identified PA patients with potentially resectable (T1-3M0) disease. Only patients resected with curative intent were included. Univariate, and multivariate logistic and Cox regression models were used to examine resection and survival. Multivariate models were adjusted for demographic factors, comorbidities, T stage, tumor size, facility type, and facility volume (20 or more resections/year = high volume).
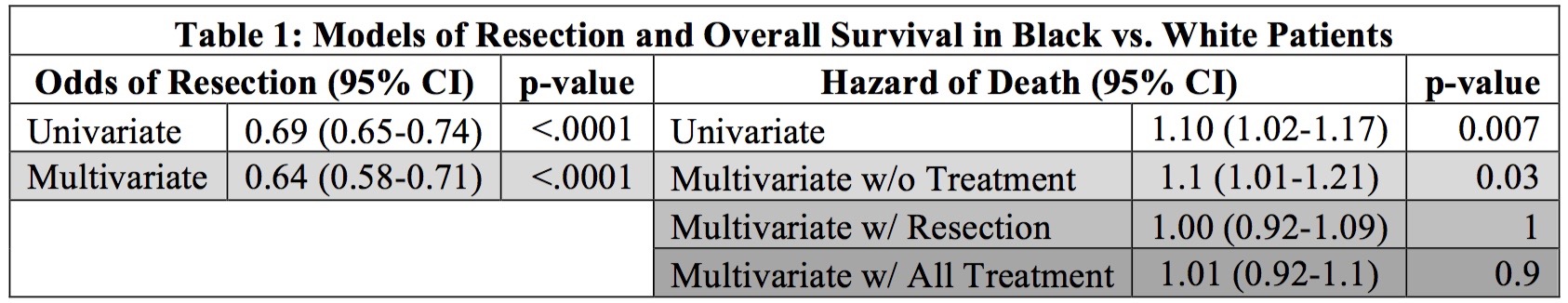
Results: Of 33,255 patients with potentially resectable disease, 3,727 (11.2%) were black and 27,908 (85.2%) were white. Black patients had lower odds of undergoing resection as compared with their white patients on univariate (OR 0.69 [95% CI 0.65-0.74, p<0.0001] and multivariable logistic regression (OR 0.64 [95% CI 0.58-0.71], p<0.0001). There was no significant difference in the refusal of surgery by race. By univariate survival analyses, resected patients survived 11.2 months longer in median survival time than unresected patients and had a lower hazard of death (HR 0.39 [95% CI 0.37-0.41], p<0.0001) while across both resected and unresected, black patients had a higher hazard of death and a reduced median survival time (HR 1.10 [95% CI 1.02-1.17], p=0.007; 9 vs. 9.66 months). This persisted in a multivariable Cox regression model that did not account for treatment factors (HR 1.10 [95% CI 1.01-1.21], p=0.03). Survival by race was similar after controlling for method of treatment (Table 1).
Conclusion: Our analyses demonstrate the importance of treating patients with resectable disease the same irrespective of race. Black patients are at much lower odds of resection as compared with white patients, but they have similar survival in multivariate models when they do undergo resection. These data highlight the importance of improving access to resection for all potential resectable PA patients.