D. H. Kim1, C. E. Cauley1, E. Fuentes1, R. Ahmad1, D. C. Chang1, D. W. Rattner1, J. T. Mullen1 1Massachusetts General Hospital,Department Of Surgery,Boston, MA, USA
Introduction: Given the epidemic of obesity and the increased incidence of gastric cancer among overweight and obese patients in the United States, it is important to understand the impact of obesity on gastric cancer surgery outcomes. Previous studies have reported conflicting results. Thus, we sought to evaluate the impact of body mass index (BMI) on both short-term postoperative outcomes and long-term survival after potentially curative gastrectomy for gastric cancer in a large, single institution cohort of US patients.
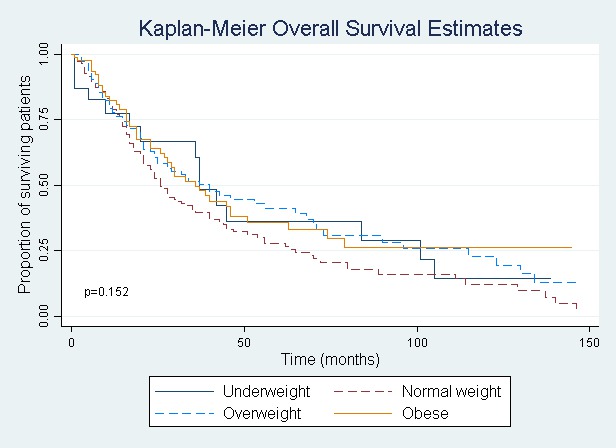
Methods: We identified 442 patients who underwent potentially curative gastrectomy for gastric adenocarcinoma between 1995 and 2014. Clinicopathologic characteristics, operative details, lymph node yield, postoperative complications, and oncologic outcomes were collected, and patients were stratified according to BMI as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5 – 24.9), overweight (BMI 25.0 – 29.9), and obese (BMI ≥ 30). We controlled for clinically relevant confounders using Cox logistic regression analysis to identify predictors of five-year mortality.
Results: Most patients had a normal BMI (n = 175, 39.6%), followed by overweight (n = 159, 36.0%), obese (n = 83, 18.8%), and underweight patients (n = 25, 5.7%). Overweight and obese patients were more likely to be young and male and to undergo esophagogastrectomy than underweight and normal weight patients, though there were no differences in tumor location, tumor stage, or extent of lymphadenectomy across groups. When stratified by BMI, there were no significant differences in the overall postoperative complication rates or in the rates of specific types or grades of complications. Specifically, there were no differences in the 30-day incidence of wound infection, anastomotic leak, or death across the BMI groups. Similarly, there were no significant differences in the length of stay or readmission rates across BMI groups. For the entire cohort, the median number of examined and positive lymph nodes was 18 and 2, respectively, and there was no difference in lymph node yield across the BMI groups. BMI was not an independent predictor of overall survival (P > 0.05) (see Figure).
Conclusion: In contrast to what many groups have previously reported, we found that BMI has no impact on postoperative complication rates, nodal yields, or long-term survival in patients undergoing potentially curative gastrectomy for gastric cancer.