L. R. Putnam1,2, K. Tsao1,2, F. Morini3, P. A. Lally1,2, K. P. Lally1,2, M. T. Harting1,2 2Children’s Memorial Hermann Hospital,Pediatric Surgery,Houston, TX, USA 3Ospedale Pediatrico Bambino Gesù,Rome, , Italy 1University Of Texas Health Science Center At Houston,Pediatric Surgery,Houston, TX, USA
Introduction:
Inhaled nitric oxide (iNO) is often used in the management of congenital diaphragmatic hernia (CDH). There is a paucity of strong evidence supporting the efficacy of iNO for CDH patients. We sought to identify the spectrum of iNO use among CDH patients and the correlation between iNO use and important clinical variables and outcomes.
Methods:
We performed an analysis of data from the international CDH Study Group registry, which comprises voluntary and prospectively collected data from over 60 international centers. We analyzed the following variables: iNO use/dose, gestational age, defect size, pulmonary hypertension (pHTN) as defined by right ventricular systolic pressure >2/3 systemic systolic pressure, operative characteristics, and extracorporeal membrane oxygenation (ECMO) use. Chi-square, Mann-Whitney U test, and regression analyses were performed.
Results:
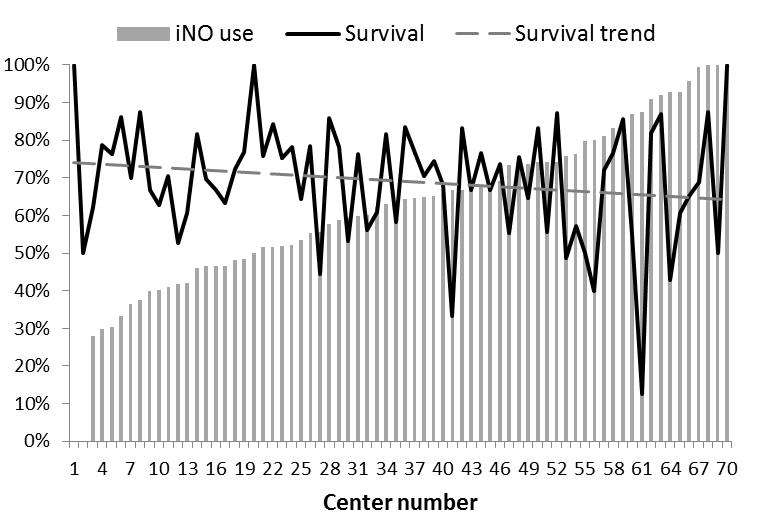
A total of 3,367 patients were identified from 2007-2015. iNO was used in 2,047 (61%) of all patients. The median (range) iNO dose was 20 (0.1-80 ppm), treatment duration was 8 (0-100 days), and day of life at initiation was 1 (0-189 days). Seventy (3%) patients received 2 iNO treatments, and 7 had >2 treatment periods. Of those patients with evaluable pHTN data (n=3117, 93%), 2,174 (70%) had pHTN, of which 1,613 (74%) were treated with iNO. Of the 943 patients without pHTN, 343 (37%) were treated with iNO. On multivariate regression analysis, iNO use was associated with worse pHTN on initial echocardiogram, larger defect size, ECMO use, and center (all p<0.05). Mean iNO use by center was 62% (0-100%) and its use was inversely associated with the trend in survival (Figure). On multivariate regression analysis, mortality was significantly associated with iNO use (OR 2.8, 95%CI 1.9-4.1), ECMO use (OR 4.1, 95%CI 3.1-5.3), and defect size (A: reference; B: OR 3.4, 95%CI 1.2-9.6; C: OR 8.9, 95%CI 3.2-25; D: OR 18, 95%CI 6.7-52).
Conclusion:
Our analysis revealed that iNO use is associated with pHTN, ECMO use, and defect size. However, we found its use highly variable among centers and over 1/3 of patients without pHTN received iNO. Without strong evidence to support its use, future studies should aim to evaluate its efficacy and standardize its application in order to optimize patient outcomes and ensure cost-effective practices.