P. E. Lau2,4, S. M. Cruz2,4, D. L. Cass1,2,4, S. E. Horne2, T. C. Lee1,2,4, S. E. Welty3, D. Lazar2,4, J. Garcia-Prats5, O. O. Olutoye1,2,4 1Texas Children’s Hospital,Texas Children’s Fetal Center,Houston, TX, USA 2Texas Children’s Hospital,Pediatric Surgery,Houston, TX, USA 3Texas Children’s Hospital,Pediatrics,Houston, TX, USA 4Baylor College Of Medicine,Department Of Surgery,Houston, TX, USA 5Texas Children’s Hospital,Section of Neonatology,Houston, TX, USA
Introduction:
Several children with severe congenital diaphragmatic hernia (CDH) require extracorporeal membrane oxygenation (ECMO) for the management of respiratory failure. Fluid restriction is typical on ECMO, and on occasion ultrafiltration (UF) is used as a rescue measure. Since early 2012, our institution established a protocol introducing the routine use of ultrafiltration on ECMO (ECMO-UF). We hypothesized that routine ultrafiltration on ECMO (ECMO-UF) is associated with better fluid management, shorter ECMO duration, improved nutritional status and ultimately better long term outcomes without compromising renal function post-ECMO.
Methods:
A retrospective review of CDH cases from January 2004 to January 2015 was conducted at a pediatric tertiary center. Neonates with CDH who required ECMO therapy were included in the analysis. ECMO-UF was started within the first 6-12 hours of ECMO initiation in the Neonatal Intensive Care Unit. Prior to this, UF use was rarely used as rescue modality (ECMO group). Outcomes of patients admitted after 2012(ECMO-UF) were compared to the ECMO group. Net fluid balance, nutritional status after 48 hours on ECMO, renal function, survival and long term pulmonary outcomes were assessed. Statistical analysis was performed using Student’s t-test and Mann-Whitney U Test for continuous measurement and Fischer’s exact for categorical measurement.
Results:
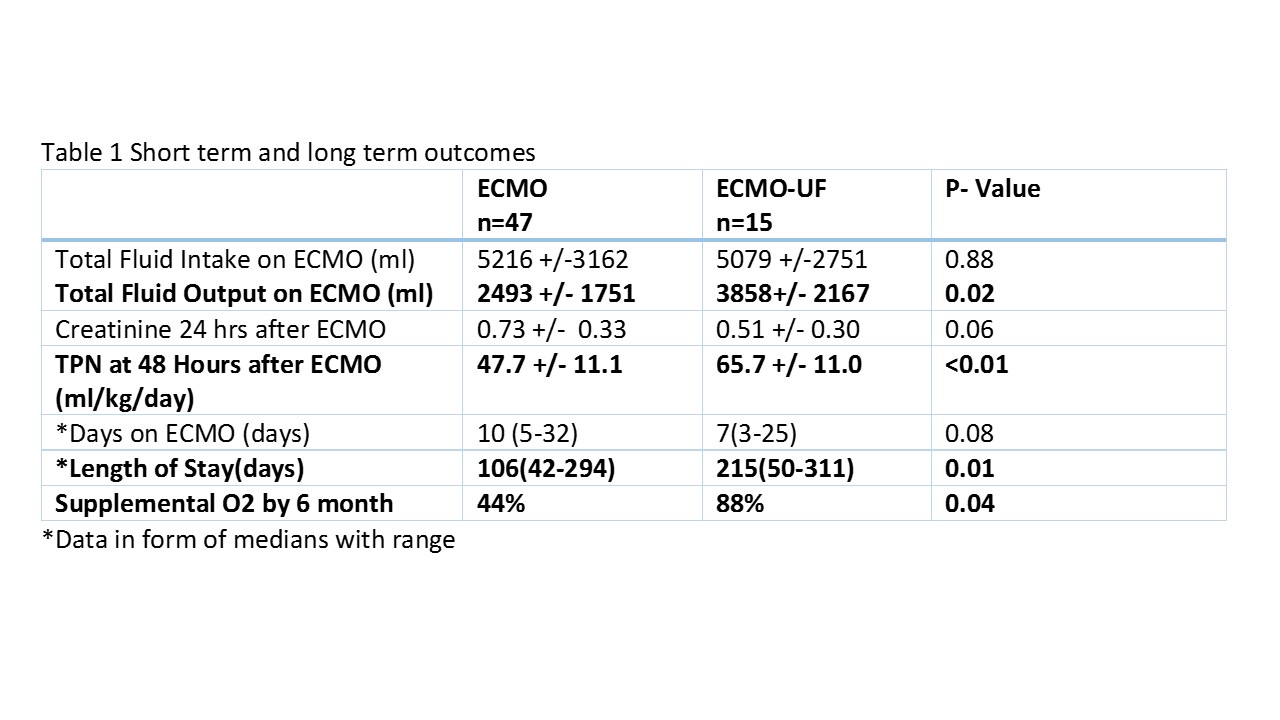
During the study period 214 CDH patients were cared for, 62 (29%) patients required ECMO. Of these, 15 (24%) had UF initiated within 6-12 hours after ECMO cannulation. Patients in the ECMO-UF group had significantly greater caloric intake with higher TPN rates at 48 hours, 47.7+11.1 vs 65.7+11 (p<0.01), and greater total fluid output on ECMO (p=0.017). There was no significant difference in renal function. No significance was seem in length of tracheal intubation, with a median number of days of 37 (20-359) in the ECMO group vs 42 (20-186) in the ECMO-UF (p=0.91). Overall 6 month survival was equivalent in both group 62.2% vs 60.9%, (p=0.25).
Conclusion:
The use of routine UF allows for better optimization of parenteral nutrition while maintaining a more favorable net fluid balance without adverse effect on renal function. Larger studies may help identify other potential benefits of routine UF in long term outcomes in infants with CDH on ECMO.