C. N. Litz1, S. M. Farach1, C. Snyder2, J. P. Jacobs2, J. Davis2, E. K. Amankwah3, P. D. Danielson1, N. M. Chandler1 1All Children’s Hospital Johns Hopkins Medicine,Pediatric Surgery,Saint Petersburg, FL, USA 2All Children’s Hospital Johns Hopkins Medicine,Cardiothoracic Surgery,Saint Petersburg, FL, USA 3All Children’s Hospital Johns Hopkins Medicine,Clinical And Translational Research Organization,Saint Petersburg, FL, USA
Introduction:
Minimally invasive repair of pectus excavatum (PE) is the current standard of care for repair of PE; however, there exists variations in the technical aspects and the clinical management. The purpose of our study was to determine practice variations and compare outcomes between two surgical services (SS) performing PE repair at a single institution.
Methods:
A retrospective review of all patients undergoing minimally invasive PE repair from July 2013 through June 2015 was performed. General admission, demographic and outcome data were collected. Patients were grouped by surgical service (SS1 vs SS2) performing PE repair and outcome measures were compared. Statistical significance was set at p<0.05.
Results:
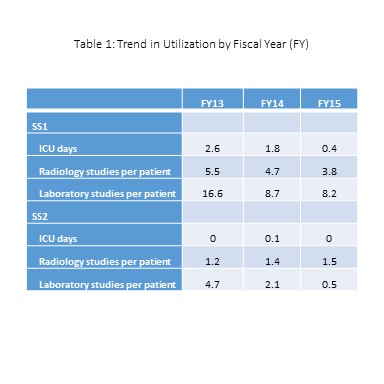
A total of 74 patients underwent PE repair during the study period (SS1 n=36, SS2 n=38). There was no significant difference in age (14.9 ± 3.7 vs 15.4 ± 2 years, p=0.494) or total hospital length of stay (3.6 ±0.8 vs 3.3 ± 1.1 days, p=0.221) between the groups. There was a significant difference in total operating room time (147 ± 24 vs 98 ± 30 minutes, p<0.001). Total charges for PE repair were significantly higher for SS1 compared to SS2 (57,579 ± 7,429 vs 40,776 ± 5,727 USD, p<0.001) as were charges for operating room services (13,577 ± 1,709 vs 4,098 ± 584 USD, p<0.001), anesthesia (3,292 ± 373 vs 2,404 ± 323 USD, p<0.001), radiology (1,399 ± 407 vs 342 ± 145 USD, p<0.001), and laboratory studies (1289 ± 801 vs 452 ± 394 USD, p<0.001). Compared to the SS2 group, patients undergoing PE repair by the SS1 group had a greater number of radiology studies (4.7 vs 1.3, p<0.0001), laboratory studies (11.9 vs 3.4, p<0.0001), and ICU days (1.7 vs 0.1, p<0.0001) per patient. Standardized practice plans were initiated with a resultant decrease in ICU, radiology, and laboratory utilization for both groups over 3 years (Table 1).
Conclusion:
There are significant variations in the surgical care of patients undergoing PE repair among surgical services, even within a single institution. Implementation of standardized practice plans help to reduce unnecessary hospital resource utilization. Recognition of these differences may provide valuable information for the purposes of improving patient outcomes while decreasing health care costs.