A. M. Stey1, C. Vinocur4, B. L. Hall3,5, M. E. Cohen3, K. Kraemer3, B. Kenney2, R. Moss2, C. Ko3,6, L. Berman4 1Mount Sinai School Of Medicine,Department Of Surgery,New York, NY, USA 2Nationwide Children’s Hospital,Columbus, OH, USA 3American College Of Surgeons,Division Of Research And Optimal Patient Care,Chicago, IL, USA 4Nemours/Alfred I. DuPont Hospital For Children,Surgery,Wilmington, DELAWARE, USA 5Washington University,Surgery,St. Louis, MO, USA 6David Geffen School Of Medicine, University Of California At Los Angeles,Surgery,Los Angeles, CA, USA
Introduction: Indications for concurrent fundoplication during gastrostomy enteral access procedures are not well established. This study aimed to determine whether 1) the propensity for concurrent fundoplication during gastrostomy varies among hospitals, and 2) whether postoperative morbidities differ significantly among institutions performing fundoplication more or less frequently.
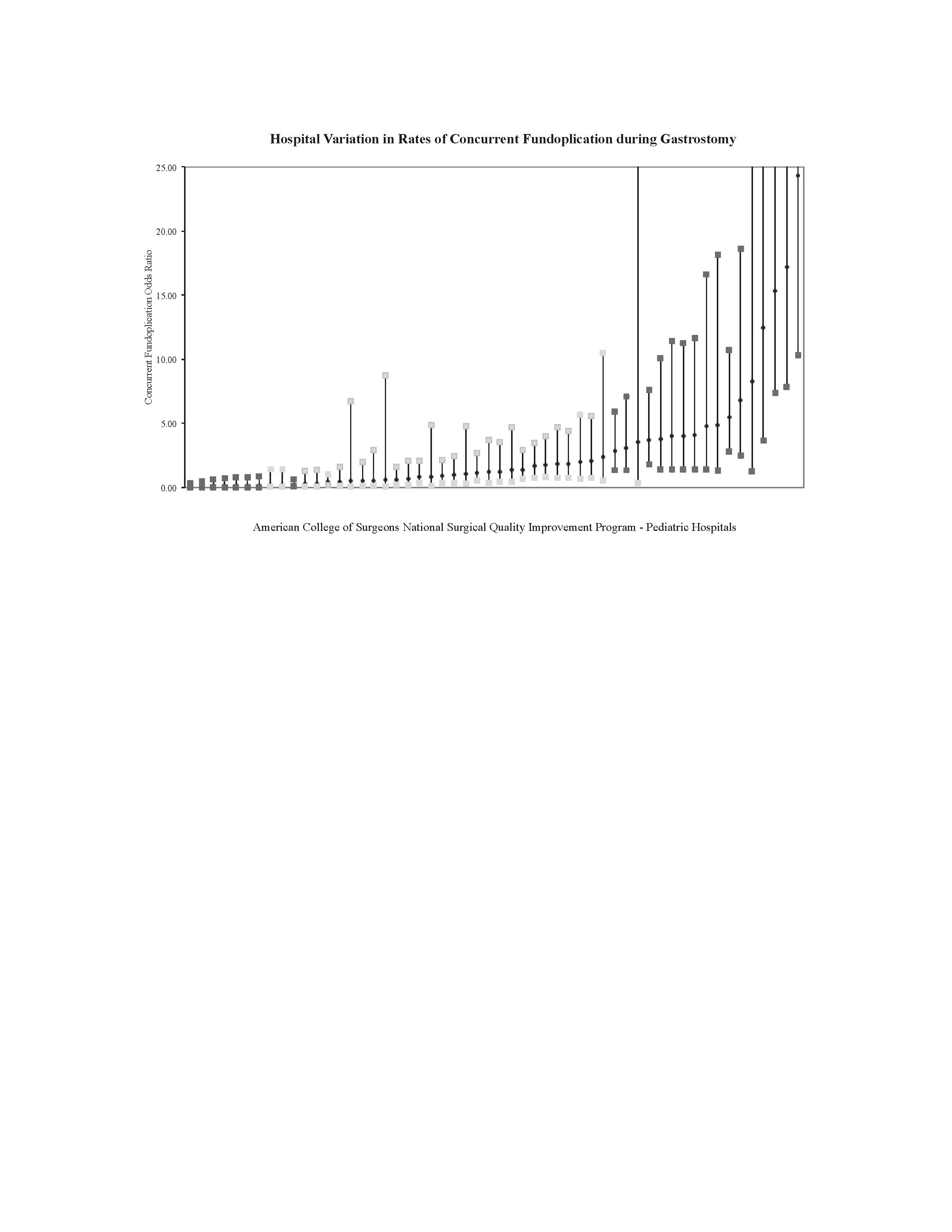
Methods: The American College of Surgeons National Surgical Quality Improvement Program Pediatric (ACS-NSQIP-P) dataset was queried to identify children who underwent gastrostomy with or without concurrent fundoplication. We created a hierarchical multivariate regression to model the propensity for concurrent fundoplication. The model included preoperative clinical variables associated with concurrent fundoplication after gastrostomy. The excess effects that hospitals exerted over the propensity of concurrent fundoplication were estimated as odds ratios. Hospitals were identified as having low, intermediate, or high odds ratios for the use of concurrent fundoplication. The risk-adjusted postoperative morbidity rates were compared among hospitals designated as low outliers, average hospitals, and high outliers in odds of concurrent fundoplication.
Results: 3,775 children underwent gastrostomy at 54 ACS-NSQIP-P participating hospitals between 2011-2013. The mean concurrent fundoplication rate was 11.7% (unadjusted range 0% to 64%). There was no significant difference in unadjusted morbidity rate in children with concurrent fundoplication, 11.0% compared to 9.7% in children without concurrent fundoplication. After controlling for clinical variables, 8 hospitals were identified as low outliers (mean observed fundoplication rate of 0.4%) and 16 hospitals were high outliers (mean observed fundoplication rate of 34.6%). The average unadjusted morbidity rate among hospitals with low, intermediate and high odds of concurrent fundoplication were 9.6%, 10.6% and 8.6% respectively (p=0.78). The added morbidity rate attributed to a concurrent fundoplication among hospitals with low, intermediate and high odds of concurrent fundoplication were 0.1%, 0.2% and 0.1% respectively (p=0.34).
Conclusion: Hospitals appear to vary significantly in propensity for concurrent fundoplication during gastrostomy in this small observational dataset yet short term morbidity did not differ significantly among the groups. These findings could demonstrate the need to clarify indications for concurrent fundoplication and the need for longer follow up to evaluate the success as well as morbidity of the procedure over time.