D. L. Lodwick1, J. N. Cooper1, K. J. Deans1, P. C. Minneci1, D. McLeod1,2 1Nationwide Children’s Hospital,Center For Surgical Outcomes Research,Columbus, OH, USA 2Nationwide Children’s Hospital,Urology,Columbus, OH, USA
Introduction: Acute testicular torsion is a surgical emergency that requires prompt diagnosis and treatment to maximize testicular salvage. Delays in care increase the chance that a patient will undergo orchiectomy rather than orchidopexy. Interhospital transfers represent a potential delay in care, and the patient and hospital level factors influencing the decision to transfer remain unclear. This population-based study aimed to determine patient and institutional factors associated with transfer for pediatric testicular torsion.
Methods: This retrospective cross-sectional study utilized the National Emergency Department Sample (NEDS) from 2006 to 2012. Encounters by males aged 1 to 21 years with one of the diagnosis codes for testicular torsion (608.2, 608.20, 608.21, or 608.22) were included. Visits at freestanding children’s hospitals were excluded. All analyses were weighted to produce nationally representative estimates. Associations of interhospital transfer with patient and institutional characteristics were evaluated using Rao-Scott chi square tests then multivariable logistic regression.
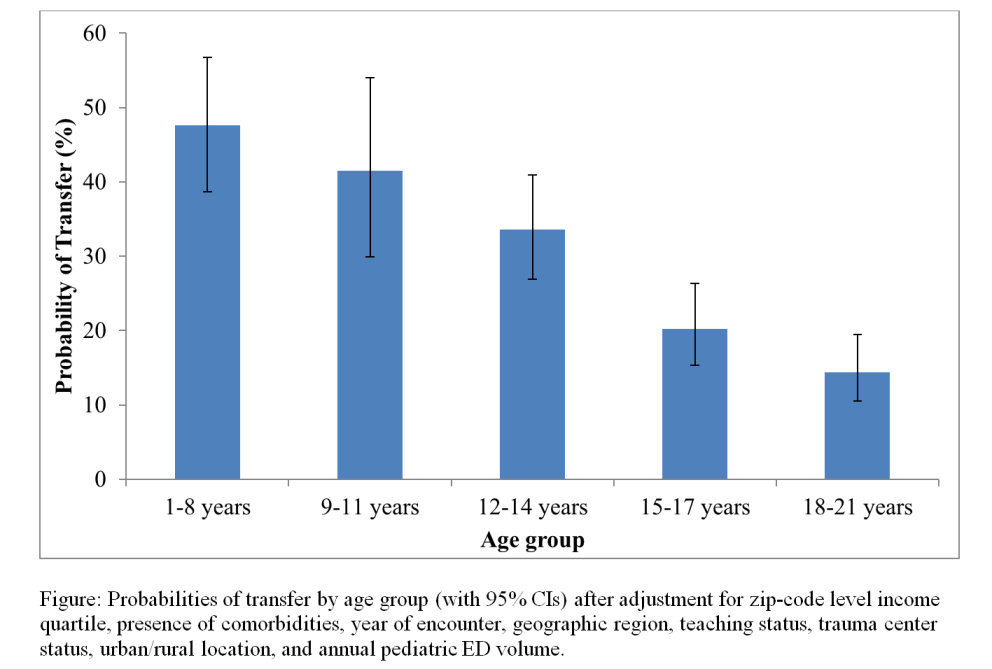
Results: During 2006 to 2012, there were 11,435 ED visits for testicular torsion by males aged 1-21 years who were either admitted or transferred to another hospital. In multivariable logistic regression, we found that the probability of transfer decreased significantly with increasing age (Figure) and was lower for patients living in zip codes in the highest income quartile (OR=0.69, p=0.003), or who had any listed comorbidity (OR=0.55, p<0.001). Patients were less likely to be transferred at hospitals in the Northeast region of the United States (OR=0.28 compared to the Midwest, p<0.001), at urban hospitals (OR=0.31, p<0.001), at teaching institutions (OR=0.55, p<0.001), and at level 1 or 2 trauma centers (OR=0.31, p<0.001). There was also a decreasing probability of transfer with increasing annual pediatric ED volume (OR=0.95 per 1000 patients seen, p<0.001). The probability of interhospital transfer increased significantly over the study period from 23.6% to 38.8% (p<0.001).
Conclusion: Older adolescents with testicular torsion are significantly more likely to be transferred than young adults. Interhospital transfers in these patients may represent a potential target for improving outcomes in testicular torsion. Future work should focus on evaluating the effect of transfer on the risk for undergoing orchiectomy.