A. K. Rzepecki1, M. Coughlin1, N. L. Werner1, H. Parmar2, M. Ladino Torres2, S. Patel2, G. B. Mychaliska1 1University Of Michigan,Pediatric Surgery,Ann Arbor, MI, USA 2University Of Michigan,Pediatric Radiology,Ann Arbor, MI, USA
Introduction: Patients with congenital diaphragmatic hernia (CDH) that require extracorporeal membrane oxygenation (ECMO) are at risk for poor neurodevelopmental outcomes. The aim of this study was to compare the head ultrasound (US) and MRI of these patients and correlate neuroimaging findings to neurodevelopmental outcome.
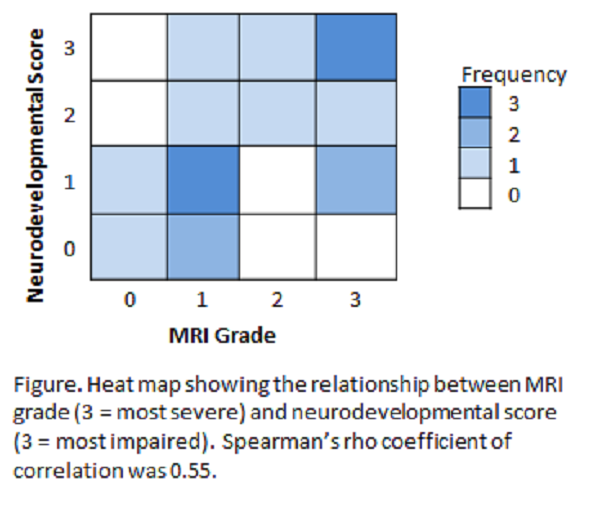
Methods: We conducted an IRB-approved retrospective review of all patients treated at C.S. Mott Children’s Hospital between 2006-2015 with a diagnosis of CDH who required ECMO. Patients were included if they had a head US and MRI in the neonatal period. Baseline patient characteristics, hospital course, and survival data were collected. Neurodevelopmental impairments were classified as 0=normal, 1=mild, 2=moderate, or 3=severe based on Peabody scores and clinical records from a multidisciplinary CDH clinic. MRIs were graded based on severity of abnormality as 0=no abnormality, 1=mild (ventricular dilation or small extra-axial hemorrhages), 2=moderate (large parenchymal hemorrhage or combination of mild hemmorrhagic and non-hemorrhagic abnormalities), or 3=severe lesions (multiple large parenchymal hemorrhage, diffuse atrophy, diffuse leukomalacia). Spearman’s rho was used to calculate a correlation coefficient between neurodevelopmental impairments and MRI grades.
Results: There were 64 patients with a diagnosis of CDH that required ECMO. 22 of these patients had both head US and MRI evaluation. The overall survival of this cohort was 77%. The defect was left-sided in 77%. The mean length of stay was 99±60 days, and the mean ventilator-free days in 60 days of life was 16±17. The mean duration on ECMO was 15±7 days. Median follow up among survivors (17/22) was 1,038 days (IQR 196-1,665). US did not demonstrate acute bleeding in any patients, but did identify dilated ventricles and prominence of extra-axial spaces in 14%. MRI of these patients also did not show significant bleeding, but found 2/22 (9%) with no abnormality, 7/22 (32%) with mild lesions, 3/22 (14%) with moderate lesions, and 10/22 (45%) with severe lesions. Neurodevelopmental impairment was mild in 6/17 children (35%), moderate in 3/17 (18%), severe in 5/17 (29%), and absent in 3/17 (18%). Spearman’s rho correlation coefficient between neurodevelopment impairments and MRI grades was 0.55 (Figure).
Conclusion: This study suggests that brain MRI and US correlate in the detection of major findings such as bleeding, however MRI is more accurate than US in detecting subtle changes such as volume loss in CDH patients that required ECMO. Correlation between MRI and neurodevelopmental outcomes was weak. These data suggest the importance of close surveillance for neurodevelopmental outcome regardless of early MRI findings.