K. W. Gonzalez1, B. G. Dalton1, K. L. Weaver1, A. K. Sherman1, S. D. St. Peter1, C. L. Snyder1 1Children’s Mercy Hospital- University Of Missouri Kansas City,Pediatric Surgery,Kansas City, MO, USA
Introduction: Extracorporeal life support (ECLS) has proven to be a lifesaving measure for patients with cardiovascular collapse. Although several studies address the uses and outcomes of ECLS, no studies have specifically evaluated the impact the time of cannulation has on clinical outcomes. We sought to compare the incidence of complications based on timing of cannulation during the work day.
Methods: A retrospective review was conducted in patients less than 18 years of age who were placed on ECLS at a pediatric tertiary care center between May 2004 and May 2015 by the pediatric general surgery service. Data analyzed included gender, age at cannulation, timing of cannulation and decannulation, total duration of ECLS, diagnosis, complication and survival to discharge. Patients placed on ECLS during the work day were compared to those placed on ECLS after hours using 2-tailed Student t-tests and Pearson chi-square.
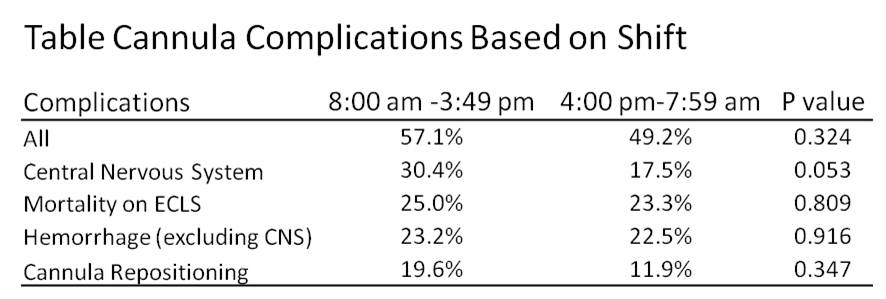
Results: There were a total of 176 patients placed on ECLS. The most common indications for cannulation were congenital diaphragmatic hernia (n=58), primary pulmonary hypertension (n=41), meconium aspiration (n=19), and respiratory failure (n=18). There was a male predominance (61%), and the median age of cannulation was 2 days (0, 5526 days). One hundred sixty two patients underwent preoperative echocardiogram; 83% of these had cardiac dysfunction, most often pulmonary hypertension. Forty one (23%) patients were placed on ECLS between the hours of 12 AM to 7:59 AM, 56 (32%) patients between 8AM and 3:59 PM, and 79 (49%) patients between 4 PM and 11:59PM (p < 0.01). When comparing scheduled operative hours (8 AM-3:59 PM) versus off hours (4PM-7:59AM), there was no statistically significant difference in total complications, central nervous system derangement, mortality on ECLS, hemorrhage (non intracranial source), or cannula repositioning (Table). Conversion from venovenous to venoarterial bypass (1.8% versus 3.4%, p=0.35) and survival to discharge (62.5% versus 60.0%, p=0.75) were also similar. The timing to decannulation was comparable (240 ± 172 hours versus 207 ± 120 hours, p=0.21).
Conclusion: More patients were placed on ECLS in the evening compared to other time frames. Despite the natural concern for the initiation of ECLS during off hours, we found no significant difference in patient outcomes.