A. Vijayasekaran1, W. Gibreel1, K. Bakri1, B. Carlsen1, M. Saint-Cyr2, B. Sharaf1 1Mayo Clinic,Plastic Surgery/Department Of Surgery,Rochester, MN, USA 2Scott & White Healthcare,Plastic Surgery,Temple, Texas, USA
Introduction:
The (Anterolateral thigh) ALT flap was initially described as a free flap but over the last decade the use of the ALT flap as a pedicled flap (PALT) for locoregional reconstruction has increased. We sought to review our institutional experience with PALT flaps and analyze the technical nuances associated with increasing flap reach.
Methods:
This is a 10 years retrospective review of PALT flaps for locoregional reconstruction at the Mayo Clinic, Rochester, Minnesota from 2005 to 2015. Patient primary diagnosis, location and size of the surgical wound, radiation treatment, medical comorbidities, and peri-operative complications are presented. Descriptive statistics are reported in the form of mean ± standard deviation (SD), median (interquartile range, IQR), or counts (percentages) when applicable. Technical considerations to improve the reach of the PALT are described.
Results:
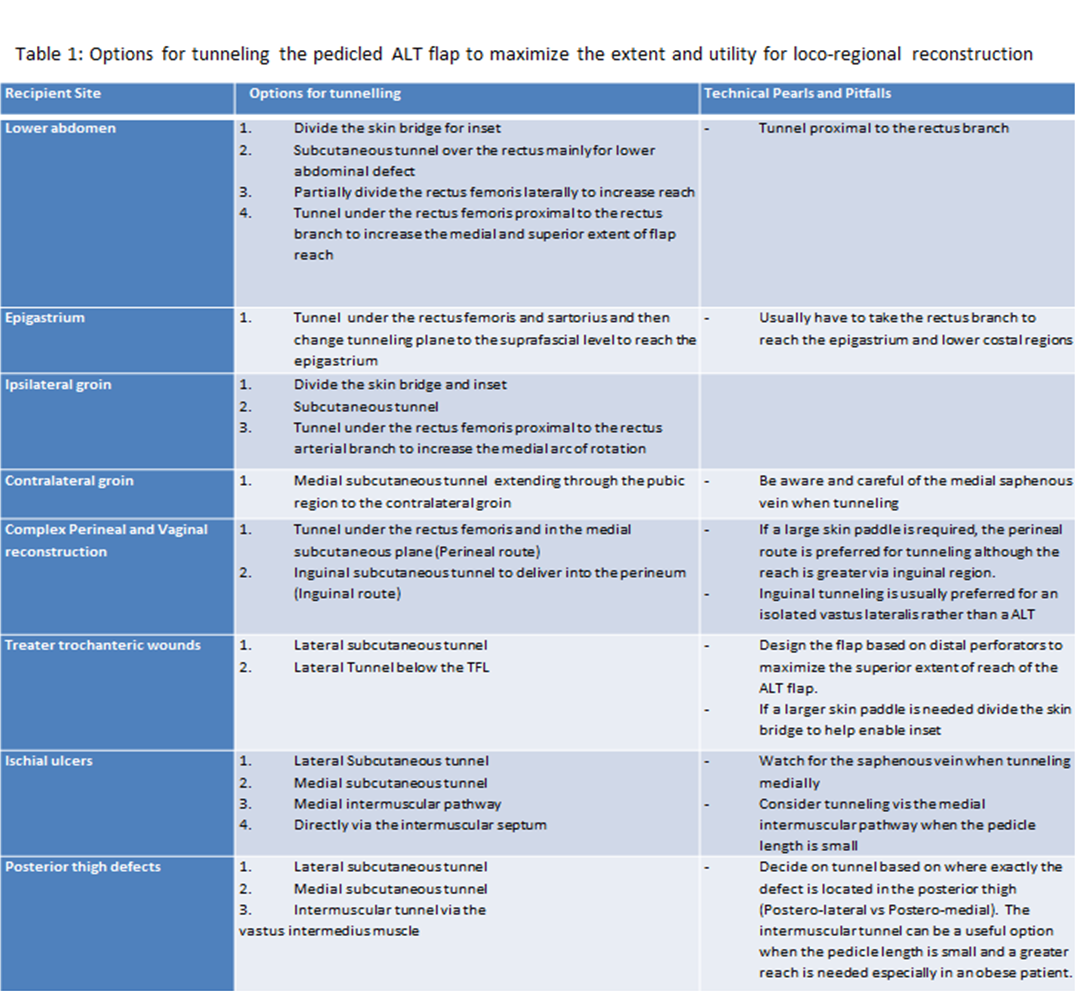
21 patients (76% males) underwent PALT flap for locoregional reconstruction. Mean duration of follow up was 20 months (range 0.4-64). Reconstruction after oncologic resection was the most common indication of PALT flap usage (n=13), followed by coverage of infected joints/prosthesis (n=8) and pressure ulcers (n=3). PALT was used for hip (n=5), groin (n=4), proximal thigh (n=3), trochanteric (n=3), lower abdomen (n=2), posterior thigh (n=2), ischial (n=1), and vaginal (n=1) reconstructions. In 28% of patients, the recipient site received pre-operative radiotherapy. A pattern of septocutaneous and musculocutaneous perforators existence in the same patients was observed in 3 patients only, the remaining 18 patients had an exclusive septocutaneous (n=9) or musculocutaneous (n=9) perforators vascular pattern. Musculo-fascio-cutaneous flaps were designed in 16 patients (4 of these were chimeric flaps), fascio-cutaneous flaps in 4 patients, and a cutaneous flap in one patient. Technical considerations to improve the reach of the PALT to cover groin, lower abdominal, perineal defects are described, including passing the flap under the rectus femoris muscle, division of the Sartorius muscle, subcutaneous tunneling of the flap, and trans-femur tunneling. The rectus femoris branch of the descending circumflex femoral artery was divided in 7 patients after confirming rectus muscle viability via clamping the vessel for 20 minutes with no evidence of any muscle necrosis. We present an algorithm to improve the reach of the PALT for various anatomic locations (Table 1).
Conclusion:
The PALT is a safe and reliable flap for locoregional reconstruction. Designing a flap with a distal skin paddle, Subcutaneous, submuscular and intermuscular tunneling and ligating the rectus branch are all technical details that help extend the reach of the PALT.