N. Provenzale1, M. Cripps1,2, T. Chung1, C. Townsend1, W. Huda1, C. T. Minshall1,2 1Parkland Health And Hospital System,Dallas, TX, USA 2University Of Texas Southwestern Medical Center,Division Of Burn, Trauma And Critical Care,Dallas, TX, USA
Introduction:
Adverse effects of blood transfusions on patient outcomes are well known; however, adherence to best practice by providers is often inconsistent. We assessed whether our transfusion practice varied respective of which primary service admitted the patient to the Surgical Intensive Care Unit (SICU). We hypothesized that average pre-transfusion hemoglobin levels for patients on elective surgery services, Otorhinolaryngology (ENT), Vascular, and general surgery, would be significantly higher than hemoglobin triggers for Emergency General Surgery (EGS) and Trauma services, despite the Surgical Intensive Care Unit (SICU) operating as a closed unit.
Methods:
The expected practice of the SICU team is to transfuse packed red blood cells (PRBCs) according to the standards established by the TRICC trial. We used a semantic layer construct to identify pre-transfusion hemoglobin levels for SICU patients between June 2014 and May 2015. Patients with uncontrolled hemorrhage were excluded. Self-service electronic health record (EHR) data reporting was used to aggregate patients by primary surgical service and retrieve medical history, BMI, and age for transfused patients. Independent samples T-tests and Fischer’s exact tests were used to assess differences between groups
Results:
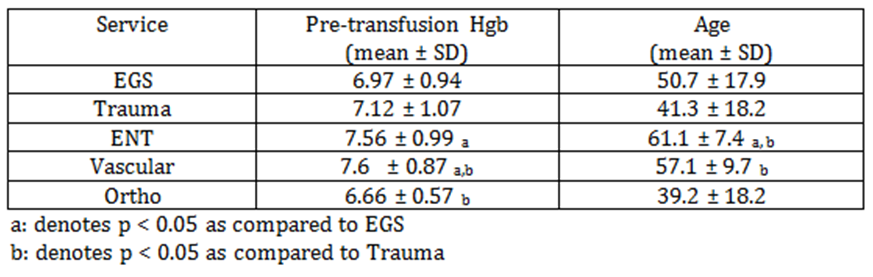
403 surgical patients were transfused ≥ 1 units of PRBCs during the study period. Average pre-transfusion hemoglobin level was significantly lower for EGS compared to the ENT and Vascular services. The average pre-transfusion hemoglobin level for Trauma was also significantly lower compared to Vascular (see Table). Two or more units were transfused in 37% of transfusion instances. EGS was the only service found to have a significant difference in average pre-transfusion hemoglobin for patients that received one unit (7.19 ± 0.28) versus two units (6.72 ± 0.44; p=0.042). The prevalence of coronary artery disease was similar between all services. ENT patients were significantly older than EGS (p=0.016) and Trauma (p<0.01) patients, while Vascular patients were significantly older than Trauma patients (p<0.01). EGS patients were more likely to have a history of diabetes mellitus as compared to both Trauma and ENT patients (p=0.01, p=0.039) and more likely than Trauma patients to have hypertension (p=0.041).
Conclusion:
This review of the transfusion practice in our SICU demonstrates variability in transfusion practice for patients on ENT and Vascular services as compared to the other services and is not justified by an increased incidence of comorbid conditions. We also have a high incidence of multiple unit transfusions. The results of this review will allow us to focus our provider education and strive to improve our performance.