R. M. Essig1, K. T. Lynch1, D. M. Long2, U. Khan1, G. Schaefer1, J. C. Knight1, A. Wilson1, J. Con1 1West Virginia University,Surgery,Morgantown, WV, USA 2West Virginia University,Biostatistics,Morgantown, WV, USA
Introduction:
‘Secondary overtriage’ refers patients discharged home shortly after being transferred to another hospital. Although minimally injured patients could potentially be discharged home, a recent regional study showed that 9.8% of these seemingly uninjured patients seen at level 3 and 4 trauma centers were transferred to a higher level of care prior to being discharged. We analyze these occurrences at the national level to identify patient characteristics and injury patterns which may facilitate the development of strategies to reduce overtriage rates.
Methods:
Data from the National Trauma Data Bank was obtained from 2008-2012 to isolate those who were: 1) discharged home within 48h of arrival, and 2) did not undergo a surgical procedure. We then identified those who arrived as a transfer to a Level 1 or 2 Trauma Center prior to being discharged (secondary overtriage) from those who were discharged directly from a Level 3 or 4 Trauma Center. Factors associated with transfer were analyzed using a logistic regression. Injuries were classified based on the need for a specific consultant. Co-morbidities examined included: smoking status, functionally dependent status, diabetes, and history of cerebrovascular accidents.
Results:
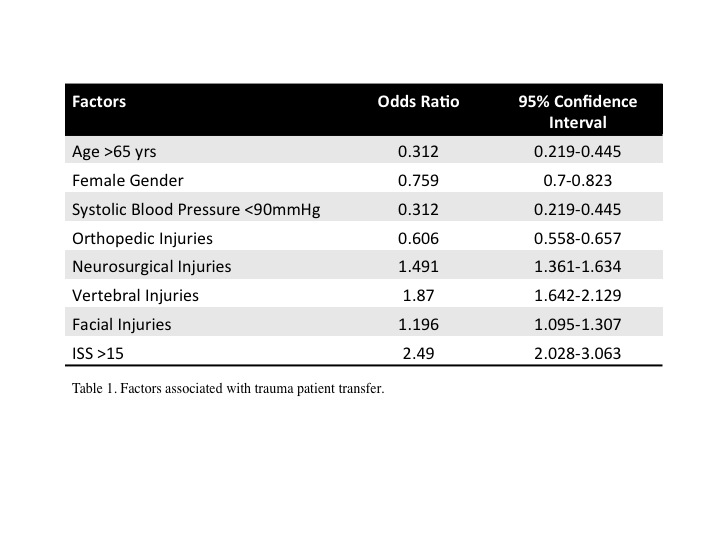
Descriptive analysis showed a number of differences between transfers and non-transfers due to our large sample size. Those who were not transferred tended to be older than 65 years (21.3% vs. 15.5%) and female (35.3% vs. 26.9%). Rates of hypotension (SBP<90mmHg) were low (0.6% vs. 1.3%) and those with ISS>15 were more likely to be transferred (10.5% vs. 3.7%). No clinically significant differences in co-morbidities were found between groups. We examined the more siginificant variables using a logistic regression controlling for age, gender, ISS, SBP<90, and injury pattern (Table 1). Neurosurgical injuries, vertebral injuries, and facial injuries were associated to an increased risk of transfer, while orthopedic injuries were protective.
Conclusion:
Secondary overtriage results from a combination of limited hospital resources, patient characteristics, and injury pattern. Although some injuries such as mild traumatic brain injuries and stable spine fractures are managed expectantly, it seems that they may be the underlying reason behind many of these transfers. A fear of an underdiagnosed or a progressing central nervous system injury may prompt a referral to a specialist for evaluation. Orthopedic injuries may involve a mechanism isolated to a single limb and therefore be considered more stable. Further studies into how these types of injuries are treated at Level 3 and 4 trauma centers may help reduce inefficiencies stemming from unnecessary transfers.