D. Laan1, T. Pandian1, D. Morris1 1Mayo Clinic,Trauma Critical Care And General Surgery,Rochester, MN, USA
Introduction: We noticed that some of our elderly patients developed swallowing dysfunction after suffering an injury. We aimed to determine the incidence of swallowing dysfunction in our elderly trauma patient population. Additionally, we wished to evaluate the clinical impact of newly diagnosed swallowing dysfunction in this group and determine risk factors for dysphagia to identify patients that might benefit from screening.
Methods: A retrospective review of our trauma database from 2009 – 2012 was conducted. Injured patients ≥75 years who had newly diagnosed swallowing dysfunction by video swallow study were identified. A comparison group without dysphagia was also identified from this time period that was frequency matched by age, gender, injury mechanism, and injury severity score (ISS). Relevant demographics and injury characteristics were collected along with patient comorbidities, complications (pneumonia, urinary tract infection, stroke, etc.), hospital length of stay (LOS), and discharge disposition. The groups were compared using Fisher’s exact tests for categorical variables and Wilcoxon rank sum tests for interval or continuous variables. Factors which reached statistical significance (p<0.05) on univariable analysis were then used to create a multivariable logistic regression model to determine independent risk factors for dysphagia.
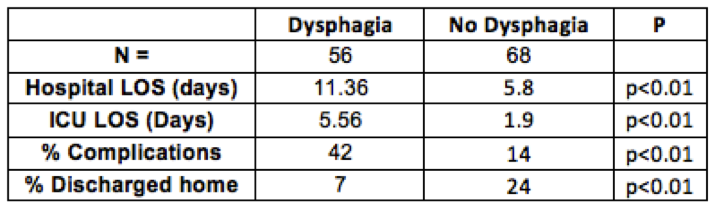
Results: In total, 1323 patients met age and injury criteria. Of these, 56 (4.2%) had newly identified swallowing dysfunction; the majority (n=38, 68%) were male. The average age and ISS were 84.38 (SD=4.54) and 11.29 (SD=6.26), respectively. The majority (85%) of patients were injured due to a fall. Comorbidities were similar between cases and controls. Regional injury patterns were also similar. On univariate analysis, patients with dysphagia had higher rates of pneumonia (15 % vs. 4 %, p<0.05), longer ICU LOS (5.6 vs. 1.9 days, p < 0.01), and longer hospital LOS (11.4 vs. 5.8 days, p < 0.01). In-hospital complication rates were higher in patients with dysphagia (42% vs. 14%, p < 0.01), and these patients had lower rate of discharge home (7% vs. 24%, p<0.01). On multivariable regression, ICU LOS was independently associated with a diagnosis of dysphagia (OR 1.46, p<0.05). All patients who had a tracheostomy were diagnosed with dysphagia.
Conclusion: Newly diagnosed swallowing dysfunction is relatively uncommon in elderly trauma patients, but the clinical implications of newly diagnosed dysphagia are important. Screening for dysphagia with swallowing study should be considered for patients with ICU LOS > 2 days or who had a tracheostomy.