A. E. Ertel1, K. Wima1, R. S. Hoehn1, D. E. Abbott1, S. A. Shah1 1University Of Cincinnati Medical College,General Surgery,Cincinnati, OH, USA
Introduction: Due to the increase in kidney transplants performed in the elderly population (>65 years old), we aimed to characterize the effects of recipient age on perioperative outcomes in the United States.
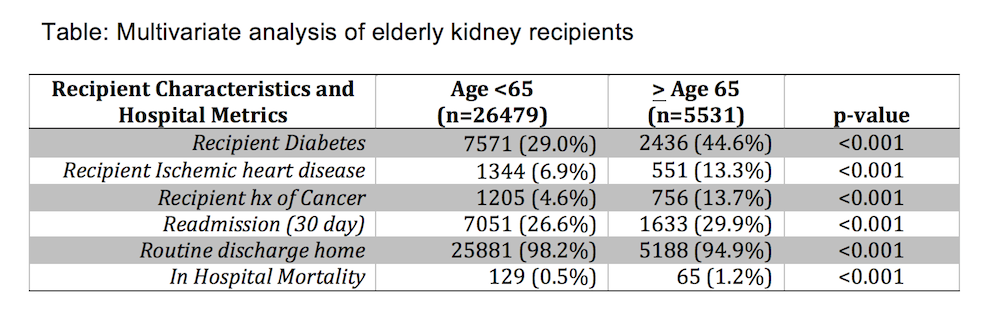
Methods: The Scientific Registry of Transplant Recipients (SRTR) was queried for all kidney transplantations from 2009-2012 and linked to the University HealthSystems Consortium (UHC) database (n=32,010). Two groups were created: recipients < 65 years (n= 26,479) and elderly recipients >65 years (n=5,531). Primary endpoints were in-hospital mortality and resource utilization metrics in the perioperative period.
Results: Compared to recipients < 65 years, elderly recipients were more likely to be white, male, have multiple co-morbidities including diabetes, ischemic heart disease, and cancer. They were more likely to receive extended criteria allografts (34.2% vs. 12.4%, p<0.001) and less like to receive living donors kidneys (28.9% vs. 41.1%, p<0.001). Elderly recipients also had a higher in-hospital mortality, readmission rate, and were less likely to be discharged to home (Table). Odds of in-hospital mortality after kidney transplant were independently associated with recipient age > 65 on multivariate analysis (OR 2.4, 95% CI 1.7-3.4), and moderate to extreme severity of illness (OR 4.1, 95% CI 1.6-10.2).
Conclusion: Elderly recipients represent 17.3% of kidney transplants in this national cohort. In-hospital mortality and resource utilization are significantly higher for elderly patients (>65) undergoing kidney transplantation as compared to their younger counterparts despite controlling for donor and recipient variables and adjusting for patient selection.