R. Sharma1, C. Ripat1, F. Pendola1, O. Picado1, D. Sleeman1,2, N. Merchant1,2, A. Livingstone1,2, D. Yakoub1,2 1University Of Miami- Miller School Of Medicine,Division Of Surgical Oncology At Department Of Surgery,Miami, FL, USA 2Sylvester Comprehensive Cancer Center,Division Of Surgical Oncology At Department Of Surgery,Miami, FL, USA
Introduction: Robotics offer improved instrumentation, precision and accuracy; it has recently been introduced to esophageal surgery. However, there is hardly any data from prospective studies to objectively evaluate its role. The aim of this systematic review was to assess the outcomes of robotic assisted esophagectomy (RAE).
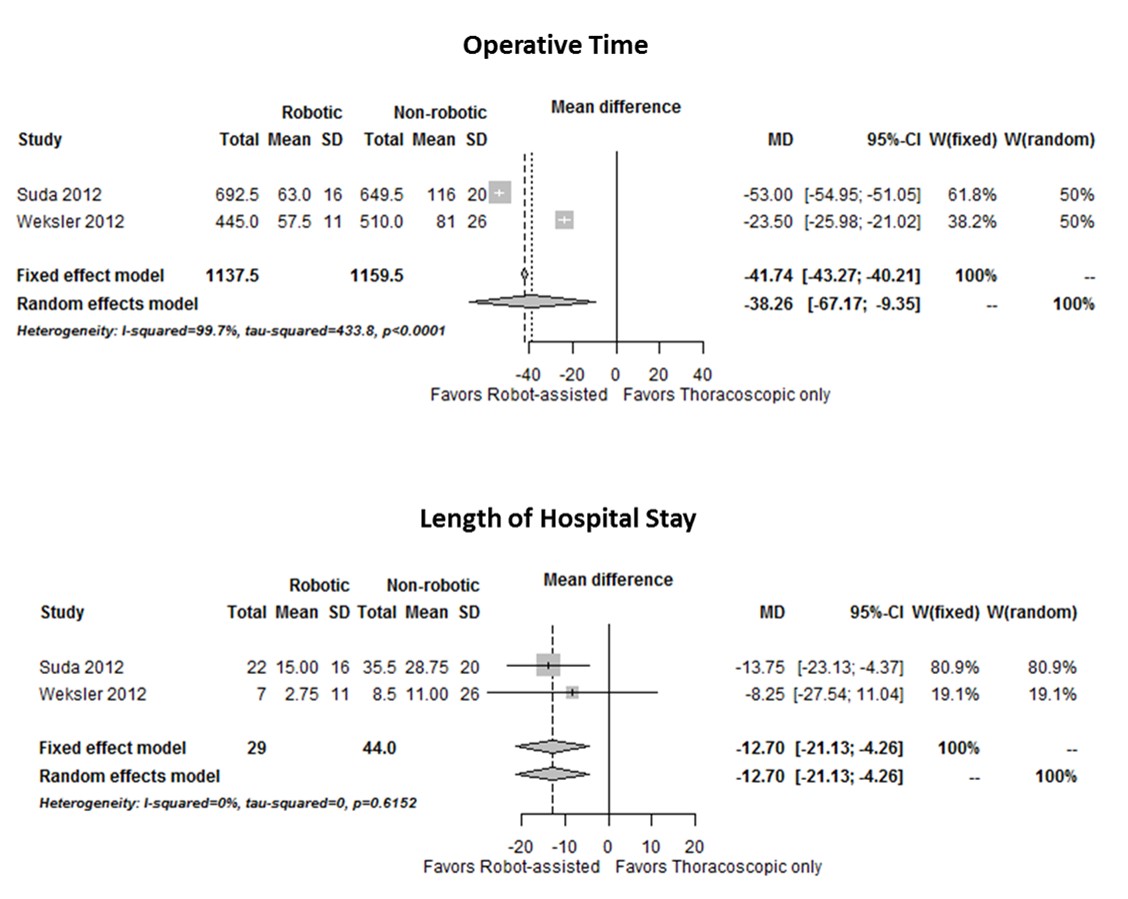
Methods: A systematic literature search was performed using Medline (PubMed), Embase, Cochrane and Scopus. Studies reporting on short and long-term clinical outcomes of RAE were reviewed. Patient demographics, tumor characteristics, surgical outcomes such as operative time, blood loss, and post-operative complications and mortality were systematically collated. For comparative studies included, meta-analysis using random and fixed effect models was done by calculation of pooled relative risk with the corresponding 95% confidence interval (CI). Study quality was assessed using STROBE criteria.
Results: Our search yielded a total of 17 studies, only two of those compared RAE with thoracoscopic technique. The studies included a total of 666 patients with esophageal cancer who underwent RAE from May 2006 to April 2015. Tumor histology was adenocarcinoma in 386 (58%), squamous cell carcinoma in 162 (24%) and other in 118 (18%). Review of all included data on RAE showed a median blood loss of 148 (R: 10-5300) ml, operative time of 410 (R: 120-807) minutes, length of hospital stay of 10.4 (R: 4-182) days, and ICU stay of 2 (R: 0-136). Median number of lymph nodes harvested was 20, (R: 3-68). 30 day mortality was (n=12, 1.8%). Complications included cardiac (0-42.9%), pulmonary (0-71.4%), vocal cord paralysis (0-37.5%), anastomotic leak (0-37.5%), wound infection (0-14.3%), and DVT/PE (0-9.5%). Meta-analysis of data from the two comparative studies showed significantly lower length of hospital stay (Mean Difference -12.7 days, 95% CI -21.1 to -4.3, p=0.003) and less operative time (Mean Difference -38.3, 95% CI -67.2 to -9.4, p=0.0095) in the RAE group. There was no difference in lymph node harvest between the two groups. Post-operative complications were less in RAE group, yet they did not reach statistical significance.
Conclusion: RAE can be performed with comparable safety and oncologic outcomes to open and thoracoscopic techniques in patients with esophageal cancer. Prospective comparative studies are needed as surgeons advance on their learning curve for using this newly introduced technology, in order to accurately evaluate the long term therapeutic and economic value of this technique.