N. N. Branch1, R. Wilson1 1Howard University College Of Medicine,Washington, DC, USA
Introduction: All who sustain open fractures may present with isolated musculoskeletal injuries or multisystem trauma putting them at risk for complications. Research is limited regarding the association between open tibia fractures and mortality; what exists suggests the two are not intrinsically linked. We sought to assess the factors which impact perioperative mortality after open reduction and internal fixation (ORIF) of isolated open tibia fractures (IOTF) using the National Trauma Data Bank (NTDB).
Methods: A retrospective analysis of the NTDB from 2007-2010 utilizing ICD-9 codes was conducted. Patients ≥ 18 years, who underwent ORIF of IOTF at a level I or II trauma centers were included. Those excluded were cases who died in the emergency department and those who were dead on arrival. Multivariate logistic regression analyzed covariates including, Glasgow Coma Scale (GCS), injury severity score (ISS), congestive heart failure, and age.
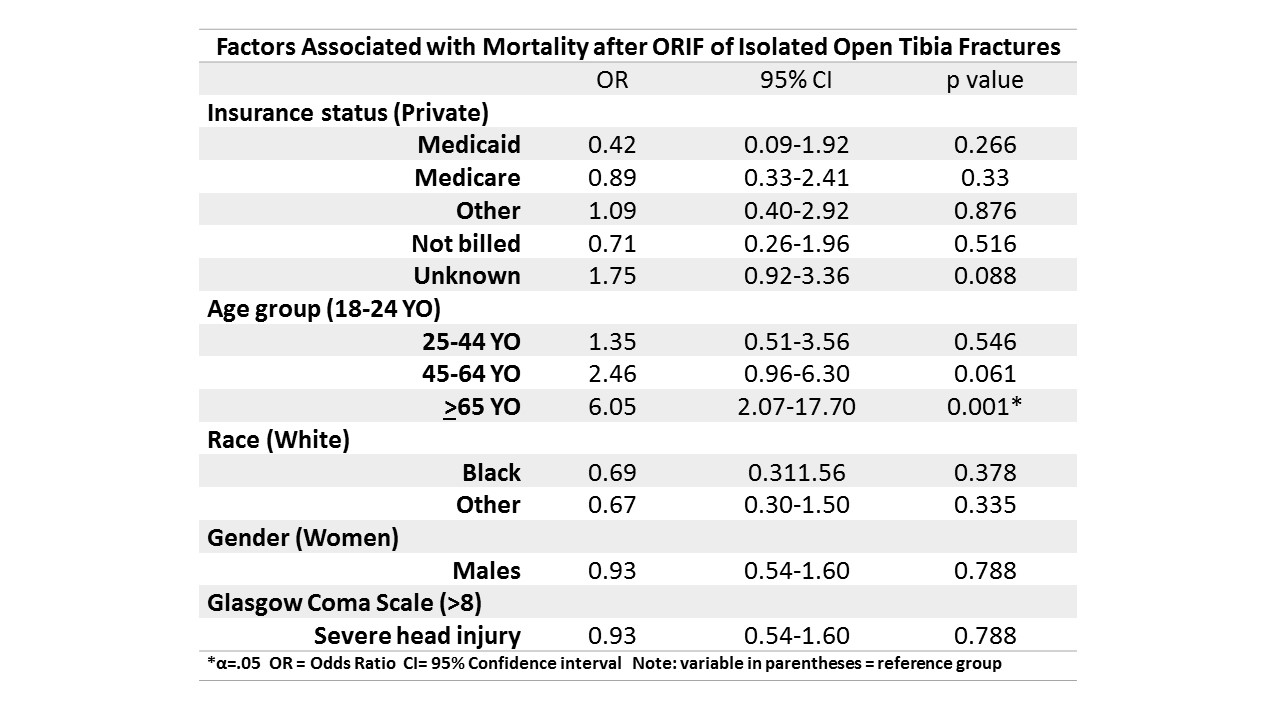
Results: 7,201 cases met the inclusion criteria. The majority were White (67%), males (74%), ages 25-44 years (42%), injured due to a motor vehicle collisions (25%), with private insurance (23%). 1.01% (n=73) of patients in our cohort died within 30 days of surgery. Among the mortalities 54 were White, 24 were female and 21 were 65 years or older. Having fixation on hospital day (HD) 1 increased odds of death (OR: 2.46 Cl: 1.05-5.78 p=0.038), compared to having fixation by HD 2. Insurance, race, gender, and GCS were not associated with perioperative death (Table 1), however the elderly were six times more likely to die (OR: 6.05 CI: 2.07-17.69 p<0.001). Patients with an ISS between 16-24 & 25-75 were five times (OR: 5.14 CI: 2.14-12.39 p<0.001) and more than nine times (OR: 9.67 CI: 4.08-22.94 p<0.001) more likely to die. Among comorbidities analyzed only those with congestive heart failure (CHF) had increased odds of death (OR: 9.32 CI: 3.00-28.94 p<0.001). Patients with any perioperative complication were almost three times more likely to die after surgery (OR: 2.9 CI: 1.57-5.36 p=0.001).
Conclusion: While the number of deaths among patients with isolated open tibia fractures was relatively small across the study period, many would argue that even one percent constitutes too many lives lost. GCS was not predictive of perioperative mortality, however, increasing ISS was predictive likely due to multisystem trauma. The elderly had a disproportionately higher odds of death compare to all other age groups. Analyzing more recent data might offer additional insight into the potential persistence of the results found here and identification of any modifiable factors to decrease perioperative death after ORIF of open tibia fractures.