L. Townsend1, M. Esquivel1, P. T. Leitz1, T. G. Weiser1, P. M. Maggio1, D. Spain1, L. Tennakoon1, K. Staudenmayer1 1Stanford University,Surgery,Palo Alto, CA, USA
Introduction: It has been estimated that 20-40% of Americans have a mental illness. We hypothesized that psychiatric diagnoses would be common in patients hospitalized for trauma in the United States and that this diagnosis would be associated with poor outcomes.
Methods: The Nationwide Inpatient Sample (NIS, 2012) was used to determine national estimates for the number of patients admitted with an injury. Psychiatric diagnoses were identified using diagnosis codes according to the Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition. Unadjusted and adjusted analyses were performed. Survey weights were used to derive national estimates.
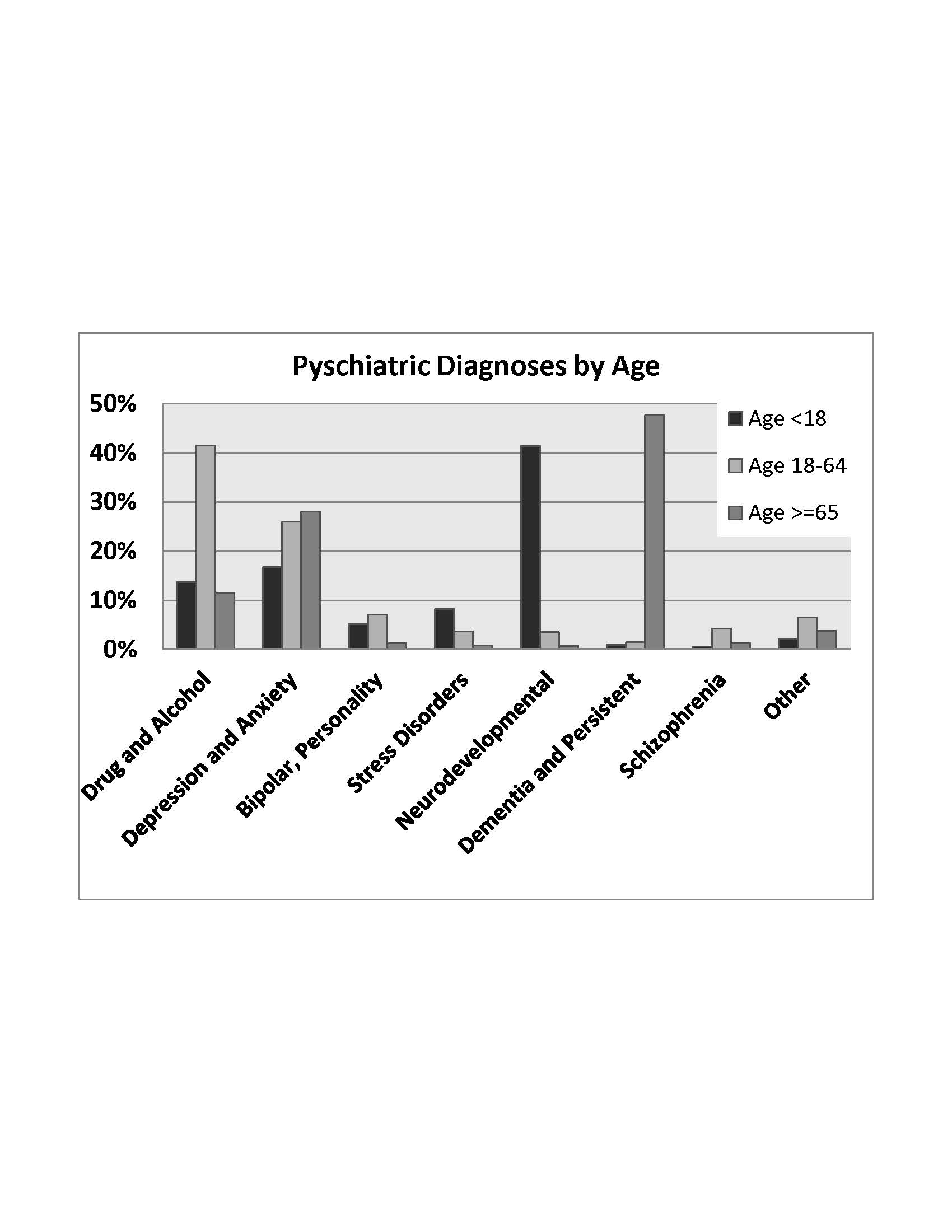
Results: A total of 1.96 million patients were admitted to hospitals in the United States in 2012 due to trauma. Of these, 861,160 (44%) had a psychiatric diagnosis. This rate was higher when compared to non-trauma inpatients (11.3 million/34.5 million, 33%, p <0.001). Psychiatric diagnoses varied by age group. For those <18 years, neurodevelopmental disorders were the most common (41%). For ages 18-64, drug and alcohol abuse predominated (41%), while dementia and related disorders (48%) were the most common in adults ≥65. Drug and alcohol abuse were common in both those <18 years (14%) and adults ≥65 years (12%). Patients hospitalized for trauma who had a psychiatric diagnosis differed in all measures compared to those without a psychiatric diagnosis. On average those with a psychiatric diagnosis were older (62 vs. 58 years, p<0.001), more often female (53% vs. 49%, p<0.001), more often white (74% vs. 68%, p<0.001), and less severely injured (mean ISS 8.8 vs. 9.6, p<0.001). Mortality was low for all trauma patients, but was lower for trauma patients that had a psychiatric diagnosis in both unadjusted and adjusted analysis (2.0% vs. 3.1%, OR 0.55, p<0.001). However, patients with a psychiatric diagnosis were more often discharged to skilled nursing care (42% vs. 32%, p<0.001) and less often to home (42% vs. 50%, p<0.001).
Conclusion: Psychiatric conditions are present in almost ½ of all hospitalized trauma patients in the United States, which is more common than what is observed in hospitalized non-trauma patients. The most common diagnosis was drug and alcohol abuse. Psychiatric diagnoses were associated with a greater number of discharges to skilled nursing facilities rather than home, suggesting an increased burden by those with a psychiatric diagnosis. The frequency of psychiatric conditions in the trauma population suggests efforts should be made to address this component of patient health to improve outcomes.