F. Gani1, J. E. Efron1, E. C. Wick1, S. H. Fang1, B. Safar1, J. Hundt1, T. M. Pawlik1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA
Introduction: The Bundled Payments for Care Improvement initiative (BPCI) was proposed by the Centers for Medicare & Medicaid Services (CMS) in an effort to obtain and reward a greater value of care. In contrast to the traditional fee-for-service paradigm, under the BPCI hospitals are reimbursed a DRG-specific bundled payment including physician and inpatient fees for a single episode of care. Still in its infancy, little is known regarding the potential effects of the BPCI on hospital payments and net margins. Therefore, this study aimed to investigate the potential effects of the BPCI on net margins among Medicare patients undergoing colectomy at a tertiary care hospital.
Methods: Medicare enrollees undergoing elective colectomy between 2009 and 2013 were identified using DRG and ICD-9-CM diagnosis codes. Total hospital costs and net payments were inflation adjusted and reported as 2013 dollars. Multivariable linear regression analysis was performed to calculate risk-adjusted, DRG-specific hospital costs and payments for each patient. Net margins were calculated as the difference between total hospital costs and total payments received.
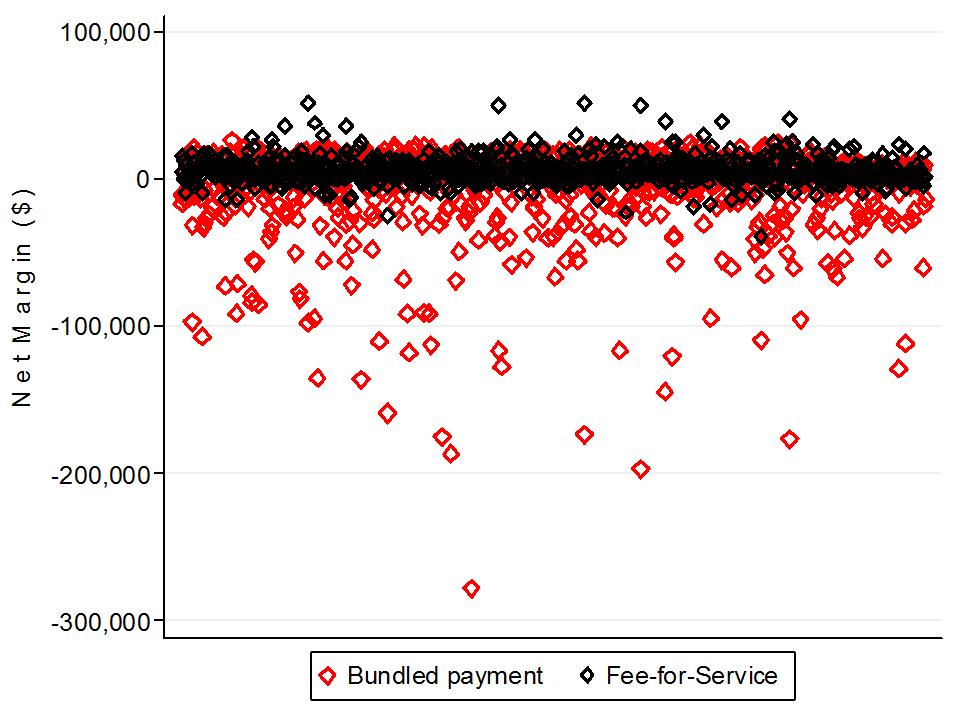
Results: A total of 821 Medicare enrollees underwent an elective colectomy and met inclusion criteria. The median age of patients was 69 years (IQR 65-74) with 48.7% being male and 67.6% presenting with one or more comorbidity. Postoperative complications were observed among 27.5% of patients. The median length of stay (LOS) was 8 days (IQR 5-14) and over a fourth of patients were discharged with additional care (27.5%). The median risk-adjusted cost among all patients was $25,202 (IQR $17,164-$42,161). Risk-adjusted costs were higher among patients who developed a postoperative complication ($43,489 [IQR $30,325-$70,885] vs. $21,179 [IQR $15,368-$32,307], p<0.001) and among patients with an Observed: Expected LOS>1 ($38,361 [IQR $26,187-$58,631] vs. $17,697 [IQR $13,414-$24,129], p<0.001). The median payment under the fee-for-service structure was $29,684 (IQR $19,609-$47,874) resulting in an overall net margin of $4,557 (IQR $1,254-$8,805), with 18.2% of patients contributing to an overall negative margin. In contrast, under the bundled payment paradigm, the net margin per patient decreased to $3,777 (IQR $-12,219-$11,825, p<0.001) with over 41% of patients contributing to a net negative margin (Figure).
Conclusions: Postoperative complications, length of stay and total hospital costs strongly correlated with hospital costs. Payments under the bundled payments system were lower and the proportion of patients contributing to a net negative margin increased. Further study is warranted to define the impact of bundled payments on quality of care, as well as hospital finances.