J. D. Bohnen1, N. F. Sangji1,2, E. P. Ramly3, H. M. Kaafarani1,2, K. D. Lillemoe1, D. C. Chang1,2 1Massachusetts General Hospital, Harvard Medical School,Department Of Surgery,Boston, MA, USA 2Codman Center For Clinical Effectiveness In Surgery,Massachusetts General Hospital,Boston, MA, USA 3Oregon Health And Science University,Department Of Surgery,Portland, OR, USA
Introduction:
Deaths among low-risk surgical patients represent an important quality improvement challenge and a potential malpractice risk. While there are many predictive models and calculators targeting overall mortality in surgical populations, a focused analysis of these ‘unexpected’ deaths may provide valuable information.
Methods:
The national ACS-NSQIP database from 2011-2012 was analyzed for all general and vascular surgery patients. NSQIP-calculated 30-day mortality risk was dichotomized at different levels, and the optimal cutoff point for ‘low’ vs. ‘high’ risk patients was established by the Youden Index, at which point the sum of sensitivity and specificity was maximized. Patients below the Youden-Index-derived mortality risk threshold were deemed low-risk (i.e. expected survivors); low risk patients who died within 30 days were considered ‘unexpected deaths’. Multivariable logistic regression models were constructed to identify perioperative predictors of unexpected deaths.
Results:
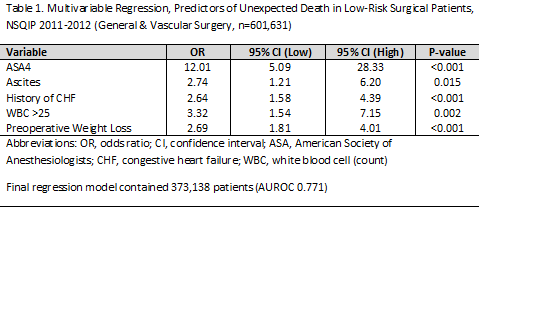
A total of 601,631 patients were analyzed. There were 8627 deaths overall (1.43%). The Youden-Index-derived cutoff point for ‘expected’ vs. ‘unexpected’ deaths occurred at a calculated pre-operative mortality risk of 1.4%. There were 994 deaths among low-risk patients (994/513702, or 0.19%), representing 11.5% (994/8627) of all deaths. In multivariable regression analyses, 19 unique variables were found to be independent predictors of unexpected deaths; the five strongest were: ASA 4 [OR=12.01, 95% CI: 5.09 – 28.33, p<0.001]; ascites [OR=2.74 (1.21 – 6.20), p=0.015]; history of CHF [OR=2.64 (1.58 – 4.39), p<0.001]; WBC > 25 [OR=3.32 (1.54-7.15), p=0.002]; preoperative weight loss [OR=2.69 (1.81 – 4.01), p<0.001].
Conclusion:
More than 11% of deaths in the surgical population occurred in low-risk patients and may be considered ‘unexpected’. The frequency and predictors of unexpected deaths provide new insights into the make-up of this unique patient group. These patients should be prioritized for directed quality improvement efforts.