A. G. Antunez1, S. K. Gadepalli1 1University Of Michigan,Pediatric Surgery,Ann Arbor, MI, USA
Introduction: Perforated appendicitis is a cause of major morbidity and reduction of rates can improve patient outcomes. Since appendicitis management is time-dependent, we hypothesized that distance and time traveled to initial evaluation and time to antibiotics impact perforation rates.
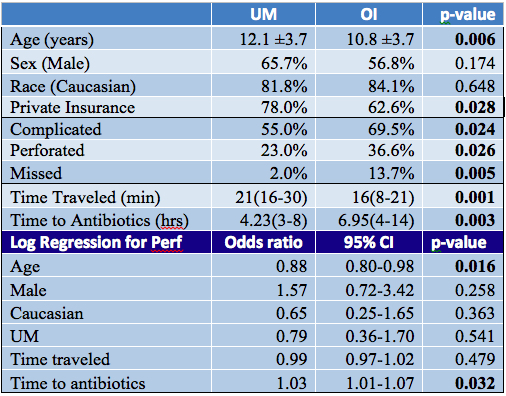
Methods: After IRB approval (HUM00095746), we retrospectively reviewed medical records, including from outside institutions (OI), of pediatric appendectomy patients from 2012-2013 at University of Michigan (UM). We collected demographics, zip codes to determine travel distances, insurance, labs, radiology, path reports, times of presentation to various institutions, to antibiotics, and to admission. We excluded patients with atypical findings not consistent with appendicitis and if over 18 years old. Primary outcome was perforated (transmural defect on path) appendicitis. Logistic regression was used to determine effect of distance and travel time and time from evaluation to antibiotics, adjusting for demographics, insurance, and site of primary evaluation with p-value <0.05 deemed significant.
Results: Of 245 appendectomies, 14 were excluded by atypical path and age criteria. Patients were 11.4±3.8yr, male (60.8%), Caucasian (83.6%), and privately insured (70.1%), with 63.2% complicated and 30.7% perforated. Interval appendectomies constituted 13.4% and diagnosis was missed previously in 8.7%. Median time traveled to initial evaluation was 18min(IQR14-25) with median distance of 11.5mi(6.8-17.4). Time for antibiotics from initial evaluation was a median of 5hr(IQR3.4-8.9). Approximately 43% were seen at UM first; there was no difference in gender and race but they were older and privately insured. Patients traveled a longer distance and took more time to be seen, but travel did not affect the rate of complicated or perforated appendicitis. Patients seen at OI first had higher rates of complicated, missed, or perforated appendicitis but received antibiotics later (p=0.003), regardless of age, race, or insurance status. On logistic regression, longer time from evaluation to antibiotics increased likelihood of perforation (OR1.03, p=0.03), when adjusted for age, race, insurance, and location of initial evaluation.
Conclusion: Distance and time traveled to initial evaluation did not increase the risk of perforation; however, the risk significantly increased with delayed antibiotic times. This study suggests that decreasing time to antibiotics during evaluation improves outcomes in pediatric appendicitis. Further prospective studies are needed to confirm our findings and determine what led to delays in antibiotic administration.