E. S. Lee1, J. S. Tieman1, J. R. Damian1, C. Martinez1, D. Boggs1, V. N. Nfonsam1, H. McClafferty2, T. Leighn3, L. A. Neumayer1, T. S. Riall1 1University Of Arizona,Department Of Surgery, College Of Medicine,Tucson, AZ, USA 2University Of Arizona,Arizona Center For Integrative Medicine,Tucson, AZ, USA 3Well Beyond Ordinary,Portland, OR, USA
Introduction: Surgeon burnout is a potential threat to the future workforce. Measuring wellbeing and teaching self-awareness during residency has the potential to decrease future burnout. The Energy Leadership Index (ELI) is an attitudinal assessment that helps individuals create self-awareness about their perceptions, attitudes, and behaviors. The ELI measures an average resonating level (ARL), which reflects their current level of self-awareness. This insight improves their ability to self-monitor and self-coach their thoughts, emotions, and behaviors in real time. Our goal was to evaluate the baseline mean and range of ARLs among surgical residents and correlate ARLs with: 1) burnout, 2) perceived stress, 3) depression, and 4) satisfaction in 14 different areas of life.
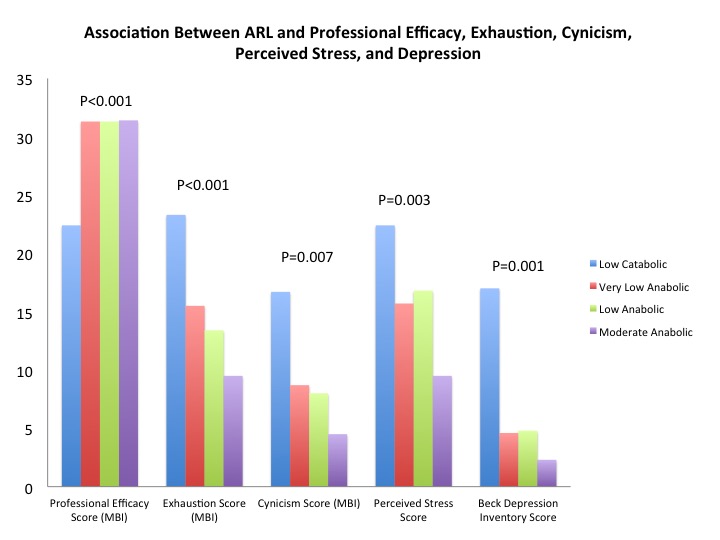
Methods: As part of a novel Wellbeing and Resiliency Program, residents at a single General Surgery Residency Program took the ELI assessment as well as the Maslach Burnout Inventory (MBI), the Perceived Stress Scale (PSS), and the Beck Depression Inventory (BDI). The ARL is reported on a 1-7 scale. Based on population-based norms for the ELI, the ARL was categorized as high catabolic (<2.50), low catabolic (2.50-2.99), very low anabolic (3.00-3.24), low anabolic (3.25-3.49), moderate anabolic (3.50-3.99), and high anabolic (≥4.0). Pearson’s R was used to measure the correlation between the ARL and the MBI, PSS, and BDI.
Results: 49 of 50 general surgery residents completed the surveys. The mean ARL was 3.16±0.24 (range 2.62-3.61). The ARL was low catabolic in 22.4%, very low anabolic in 32.7%, low anabolic in 36.7%, and moderate anabolic in 8.2% of residents. Increasing ARL was positively correlated the MBI professional efficacy score (R=0.63, p<0.001), and negatively correlated with the MBI exhaustion score (R=-0.54, p<0.001), the MBI cynicism score (R=-0.43, p=0.007), the PSS score (R=-0.36, p=0.03), and the BDI score (R=-0.54, p=0.001). Means across ARL categories are shown in the Figure. Fewer than 30% of surgical residents were satisfied with work-life balance (10.2%), time management (20.4%), health and wellness (22.4%), energy levels (24.5%), and feelings of personal freedom (28.6%). Higher ARLs were associated with satisfaction in leadership ability (p=0.03), work relationships (p=0.006), personal freedom (p=0.03), and spiritual wellbeing (p<0.001).
Conclusion: Our data demonstrate a need to improve resident wellbeing. Lower ARLs on the ELI were correlated with increased symptoms of burnout, increased perceived stress, and increased depression scores. Since professional coaching interventions have been shown to improve ARLs, a formal ELI-based coaching program has the potential to improve resident wellbeing.