M. A. Alvarez1, S. M. Husain1, L. F. Reed1, P. V. Dickson1,2, J. L. Deneve1,2, D. Shibata1,2, E. S. Glazer1,2 1University Of Tennessee Health Science Center,Memphis, TN, USA 2UT West Cancer Center,Memphis, TN, USA
Introduction: In pancreatic adenocarcinoma (PDAC), TGF-ß is a tumor suppressor known to drive inflammation in the tumor microenvironment (TME). The role of tumor associated macrophages and interleukins in the PDAC TME is not well described though both likely play critical roles. We hypothesized that pre-treatment of a primary PDAC cell line, Panc-1, with combinations of TGF-ß, macrophages, or IL23, would result in variations in tumorigenesis and metastases in an orthotopic murine model.
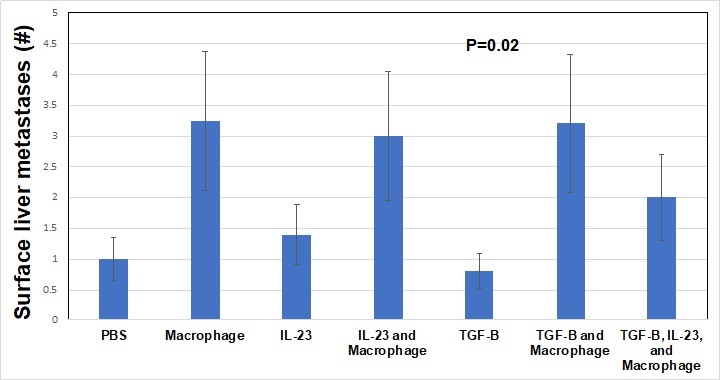
Methods: Panc-1 cells, a line derived from primary pancreatic cancer, were pre-treated with TGF-ß alone (10 ng/mL), IL23 alone (10 ng/mL), macrophages (ATCC cell line, 10:1 ratio of Panc-1 cells to macrophages), IL23 + macrophages, TGF-ß + macrophages, or TGF-ß + macrophages + IL23. Control cells were treated with PBS. Cells were treated twice weekly for 1 week in complete media then implanted into the pancreas of NOD scid gamma mice (NSG, severely immunocompromised) with 5 mice per group. Mouse weights were taken twice weekly for 4 weeks. At that point, mice were sacrificed and tumors harvested. We investigated mouse weight, pancreas tumor weight, pancreas tumor diameter, and the number of surface hepatic metastases. Mean values were compared with ANOVA.
Results: Throughout the study, the mean weight of the mice in the TGF-ß alone and IL23 alone treatment groups was stable whereas all other mice increased weight by 10% (P<0.001). Pancreatic tumor weights were highest in macrophage treatment groups. TGF-ß + macrophage treatment decreased the tumor weight compared to macrophage treatment alone (P<0.001). Macrophage treatment of Panc-1 cells was associated with the highest number of surface liver metastasis after implant (>3 per mouse) and TGF-ß treatment alone was associated with the least number of surface liver metastasis (<1 per mouse, P<0.01). Importantly, TGF-ß treatment did not modulate the rate of macrophage induced surface liver metastasis, but IL23 + macrophage + TGF-ß treatment did result in fewer surface liver metastasis compared to macrophage treatment alone (> 3 vs 2 per mouse, overall P=0.02). Macrophage treated Panc-1 cells were associated with the largest primary Panc-1 tumor growth after 4 weeks, TGF-ß treatment diminished the effect the macrophages had on the Panc-1 cell primary tumor growth (P<0.001).
Conclusion: We found that macrophages drive the development of metastases in this model of early PDAC. While other research groups have shown that TGF-ß is associated with survival in PDAC, we demonstrated that macrophages play a critical role in early PDAC and likely modulate the TME through interleukins such as IL23 and TGF-ß.