A. B. Crocker3, A. Zeymo2,3, D. Xiao3, L. B. Johnson4, T. DeLeire5, N. Shara2,4, W. B. Al-Refaie1,2,3 1MedStar-Georgetown University Medical Center,Department Of Surgery,Washington, DC, USA 2MedStar Health Research Institute,Washington, DC, USA 3MedStar-Georgetown Surgical Outcomes Research Center,Washington, DC, USA 4Georgetown-Howard Universities Center For Clinical And Translational Science,Washington, DC, USA 5Georgetown McCourt School Of Public Policy,Washington, DC, USA
Introduction: Pre-Affordable Care Act (ACA) Medicaid expansion has preferentially increased utilization of elective inpatient procedures. However, the impact of the ACA on such elective and preference-sensitive procedures (also known as discretionary procedures) vs. clinically essential and time-sensitive non-discretionary procedures remains unknown. We hypothesize that the ACA’s expansion led to increased utilization of inpatient discretionary procedures (DP) relative to non-discretionary surgical procedures (NDP) in expansion vs. non-expansion states. As such, we performed hospital-level quasi-experimental evaluations to measure the state-by-state differential effects of the ACA’s Medicaid expansion on utilization of DP vs. NDP.
Methods: The State In-Patient Database (2012-2014) yielded 476 hospitals providing selected DP or NDP procedures performed on 275,131 non-elderly, adult patients (ages 18-64 years) across three expansion states (Kentucky, Maryland, and New Jersey) vs. two non-expansion control states (Florida and North Carolina). DP included non-emergent total knee arthroplasty and total hip arthroplasty, while NDP included a cohort of nine cancer surgeries. Mixed Poisson interrupted time series (ITS) analyses were performed to determine the impact of ACA’s Medicaid expansion on the number of DP vs. NDP provided: 1) across expanded versus non-expanded states overall, 2) among non-privately insured patients (Medicaid and uninsured payers).
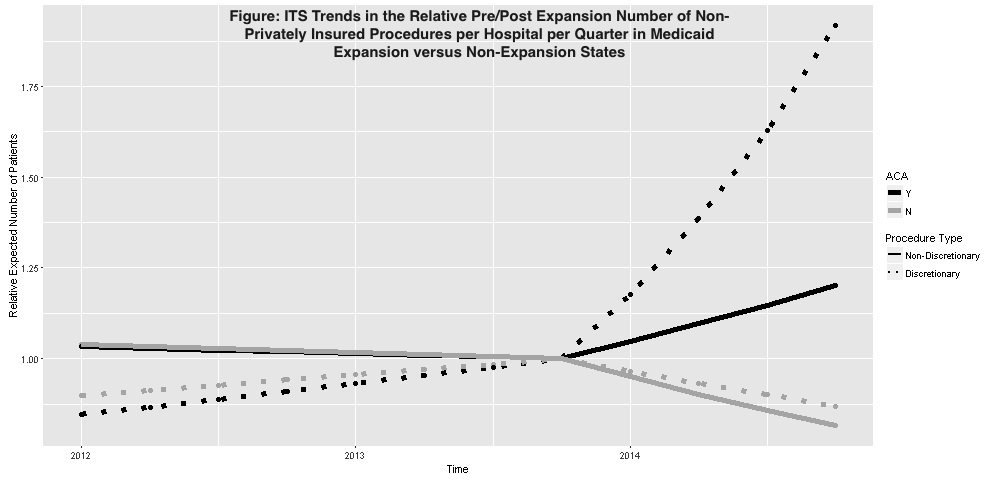
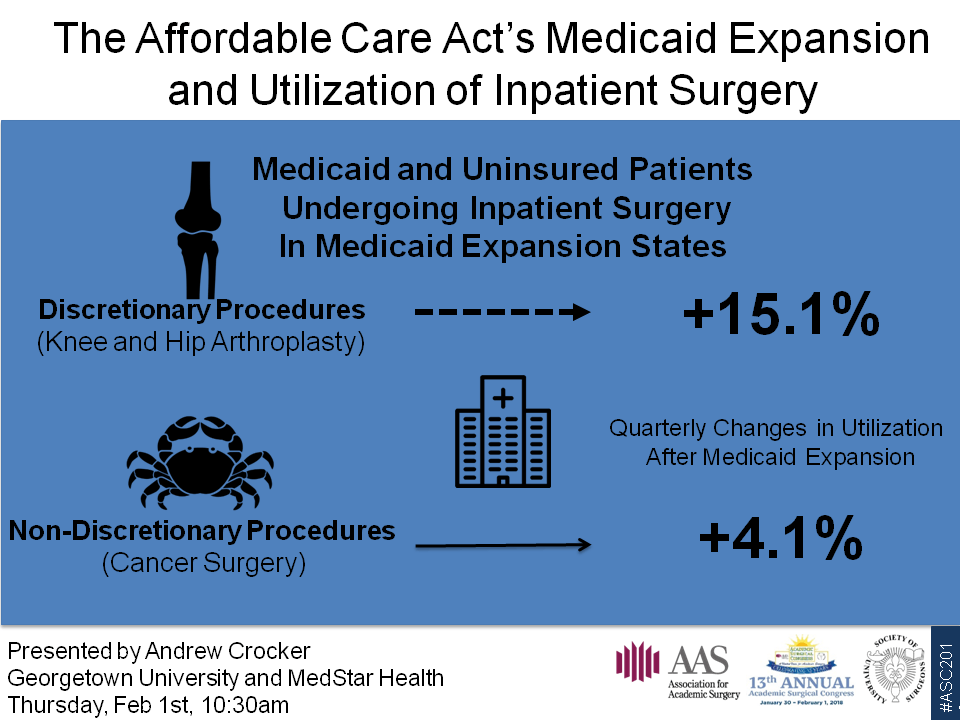
Results: Substantial reductions in the number of uninsured DPs were observed in both expansion (-73%) and non-expansion states (-45%). While the number of Medicaid insured DPs in expansion states nearly doubled, the number of privately insured DPs in non-expansion states increased by 10%. Observing no overall differential increase in the utilization of DPs in expansion and non-expansion states after 2014 (2.2% per quarter and 2.8% per quarter), subsequent analysis on the mean number of non-privately insured DP and NDP was performed. Mixed ITS estimated a differential increase in DP (+17.7% vs -3.5%) and NDP (+4.7% vs -5.0%) in expansion states compared to non-expansion states. Additionally, a substantially larger increase in utilization of DP vs NDP was detected within expansion states after 2014 (Figure).
Conclusion: In this multi-state evaluation, ACA’s Medicaid expansion has preferentially increased utilization of DP in expansion vs non-expansion states among non-privately insured patients. This expansion has also differentially increased utilization of DP relative to NDP in expansion states. These preliminary findings suggest that expansion coverage increased use of inpatient surgery. Further research is merited to expand on these early results.