B. Hewitt1, J. W. Chung1, A. R. Dahlke1, A. D. Yang1, K. E. Engelhardt1, E. Blay1, J. T. Moskowitz2, E. O. Cheung2, F. R. Lewis3, K. Y. Bilimoria1 1Northwestern University,Surgical Outcomes And Quality Improvement Center,Chicago, IL, USA 2Northwestern University,Osher Center For Integrative Medicine,Chicago, ILLINOIS, USA 3American Board Of Surgery,Philadelphia, PENNSYLVANIA, USA
Introduction: Despite great interest in resident wellness, little is known about actual rates of resident burnout as current data are limited by poor response rates, small sample sizes, or use of non-validated measures. Surgical residents are hypothesized to be at particular risk for burnout and poor well-being. We used novel national survey data with responses from nearly all U.S. general surgery residents to (1) examine burnout and poor well-being prevalence and (2) identify factors associated with burnout and well-being.
Methods: All general surgery residents were surveyed (99% response rate) at the time of the January 2017 American Board of Surgery In-Training Examination (ABSITE) regarding wellness, duty hour violations, preparation for residency, and occupational safety. The main resident wellness outcomes were burnout (abbreviated Maslach Burnout Inventory – 6 items) and psychiatric well-being (General Health Questionnaire-12 which identifies those at risk for non-psychotic psychiatric illness). Hierarchical logistic regression analyses were performed to examine resident and program factors associated with burnout and well-being.
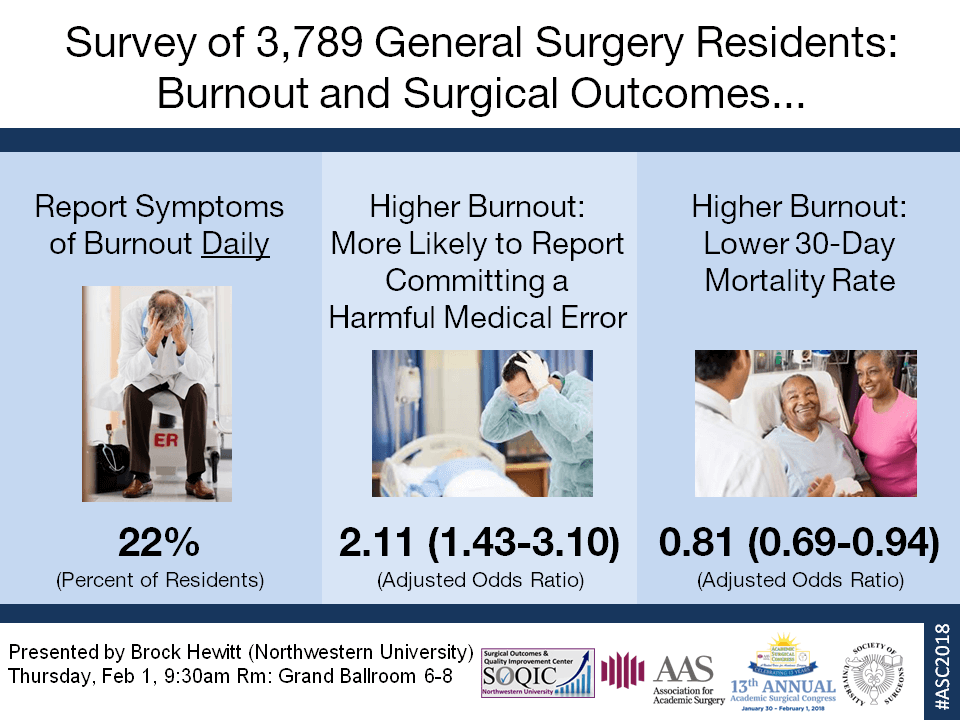
Results: Of 7,441 residents offered the survey, 7,387 residents (99.3%) in 260 surgical residency programs completed all items related to resident wellness. Overall, burnout was reported in 23.8% (n=1,756) of residents and poor psychiatric well-being in 44.3% (n=3,270). From the burnout assessment, 16.0% (n=1,184) of residents responded that they “do not really care what happens to some patients” at least a few times a month, and 18.1% (n=1,337) of residents responded that they daily “feel fatigued in the morning having to face another day on the job.” In multivariable models, burnout was more likely among male residents (OR 1.15 [95% CI 1.01-1.31]), those who felt unprepared for residency (OR 1.65 [95% CI 1.44-1.90]), and those who violated the 80 hour weekly average duty hour limit (violations in 1-4 of the past 6 months: OR 1.54 [95% CI 1.35-1.77]; violations in ≥5 months: OR 2.35 [95% CI 1.80-3.07]) compared to no violations. Burnout was not significantly associated with post graduate year (PGY). Poor psychiatric well-being was associated with similar factors with the exception of female residents (OR 1.25 [95% CI 1.12-1.38]) and PGY 1 residents (OR 1.19 [95% CI 1.04-1.35]) compared to PGY 4/5 residents who were more likely to report poor psychiatric well-being. There was no significant difference in burnout or psychiatric well-being between the Flexible and Standard arms of the FIRST Trial.
Conclusion: In this national survey including 99% of clinically active surgical residents in the U.S., burnout and poor psychiatric well-being were prevalent in surgical residents and more likely in residents who reported feeling unprepared for residency and those who violated duty hour limits. Solutions to improve resident wellness are needed and should address these associated factors.