A. M. Mechler-Hickson1, M. Gowda1, S. L. Thibeault1 1University Of Wisconsin,Department Of Surgery, Division Of Otolaryngology – Head And Neck Surgery,Madison, WI, USA
Introduction:
The larynx is of vital importance in humans, contributing to breathing, swallowing, and phonation. It is also uniquely positioned at both the junction of the respiratory and GI tracts and the immunological boundary between the upper and lower respiratory systems. Due to their position, the vocal folds (VF), which are housed in the larynx, are exposed to a wide array of inhaled and ingested challenges. There is evidence that cells in the VF play a role in responding to these challenges: TLR1-6, TLR8 and TLR9 have been found in VF fibroblasts, the primary cell type of the lamina propria. Additionally, the majority of VF diseases are inflammatory in nature and have large economic and social consequences for patients. Despite the importance of the VF, and the inflammatory etiology of much of VF disease, mechanisms of host immunity in the larynx are ill-defined, and treatment of these inflammatory disorders is largely empiric. We worked to characterize toll-like receptors (TLR) 1-9, integral receptors in the innate immune system, in murine VF tissue, as mice are frequently used as a model species for humans, and in human VF epithelial cells.
Methods:
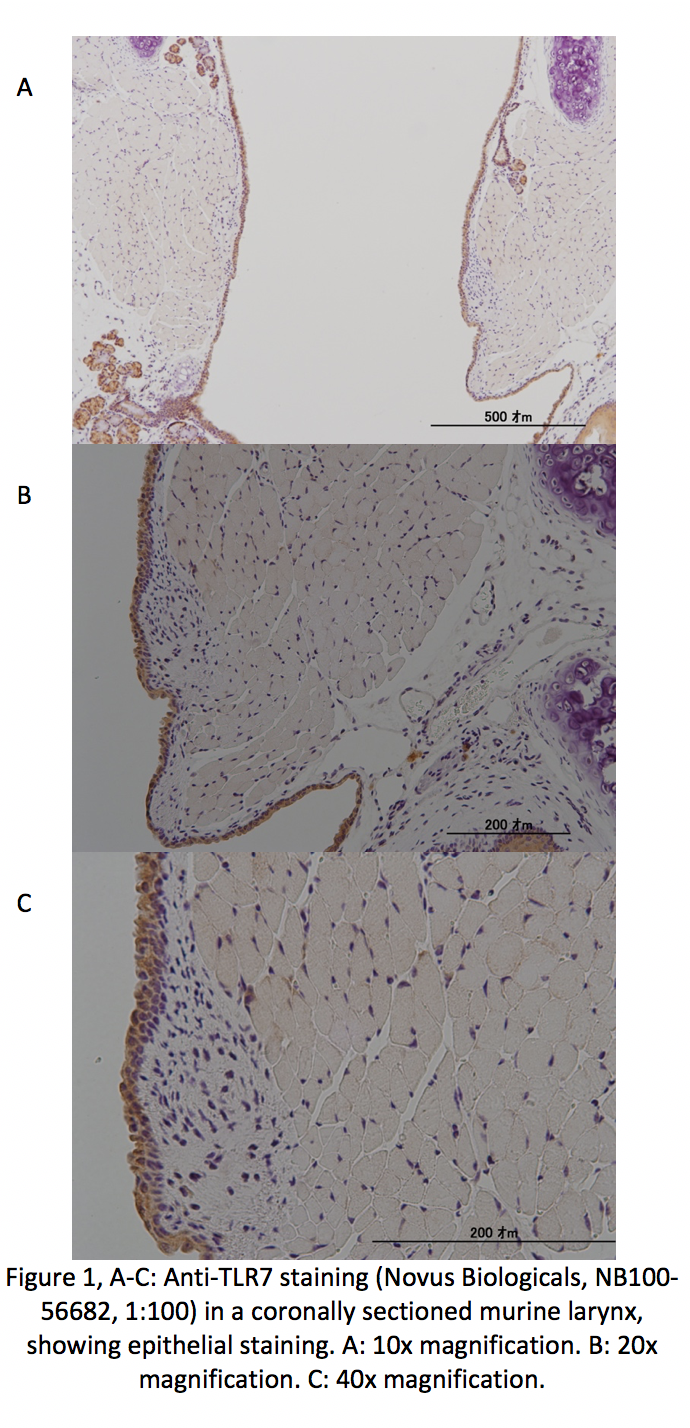
In order to localize TLR1-9 in murine VF tissue, excised larynges were coronally sectioned and processed for immunohistochemistry. Primary antibodies against TLR1-9 were used. An α-IgG secondary antibody was then applied, and diaminobenzidine was used as a staining agent. Staining was completed in biological and technical triplicate for each of the 9 antibodies with positive and negative controls.
Transcript levels of TLR1-9 were investigated in immortalized human VF epithelial cell lines. Cells were seeded into 6-well plates at a density of 1.5E5/mL and grown to near confluence. Cells were then treated with or without 5μg/mL LPS for 24 hours in wells intended for RT-PCR, and with or without 5μg/mL LPS for 8 hours in wells intended for ELISA analysis of IL-8, a downstream product of TLR activation. RT-PCR and ELISA were performed in biological and technical triplicate.
Results:
TLR1-9 were found in the epithelial cell layer of VF (Fig. 1). At the time of abstract submission results are ongoing, but we expect to find TLR1-9 in VF epithelial cells, with decreased expression for TLR6 -7. When treated with LPS we expect to find increased TLR expression and IL-8 levels, similarly to prior work in VF fibroblasts.
Conclusion:
This study localized TLR1-9 in VF epithelium. Exploring this, and how TLR expression and downstream cytokine activation differs between normal epithelial cells and those exposed to inflammatory stimuli, better elucidates how laryngeal epithelium responds to the variety of insults it is exposed to and may provide targets for treatment of airway disease.