R. R. Sheldon1, M. Loughren1, C. Marenco1, K. Morte1, W. S. Do1, D. T. Lammers1, J. B. Weiss1, D. M. Forte1, V. Y. Sohn1, M. J. Martin1, M. J. Eckert1, R. O. Burney1, S. T. Marko1, J. Bingham1 1Madigan Army Medical Center,Tacoma, WA, USA
Introduction: Microdermal implants are an increasingly popular form of body jewelry in which the device is surgically implanted beneath the skin and held in place by scar tissue that forms around the dermal anchor. The potential for electrical conduction burn at the site of metal jewelry left in situ during electrosurgery prompted surgical societies to recommend routine removal. However, routine removal of microdermal implants can be complicated, requiring destruction of the device or local excision. Given the paucity of evidence regarding electrosurgical burn risk associated with microdermal implants, we assessed in vivo thermal effect and tissue damage at implants during electrocautery use.
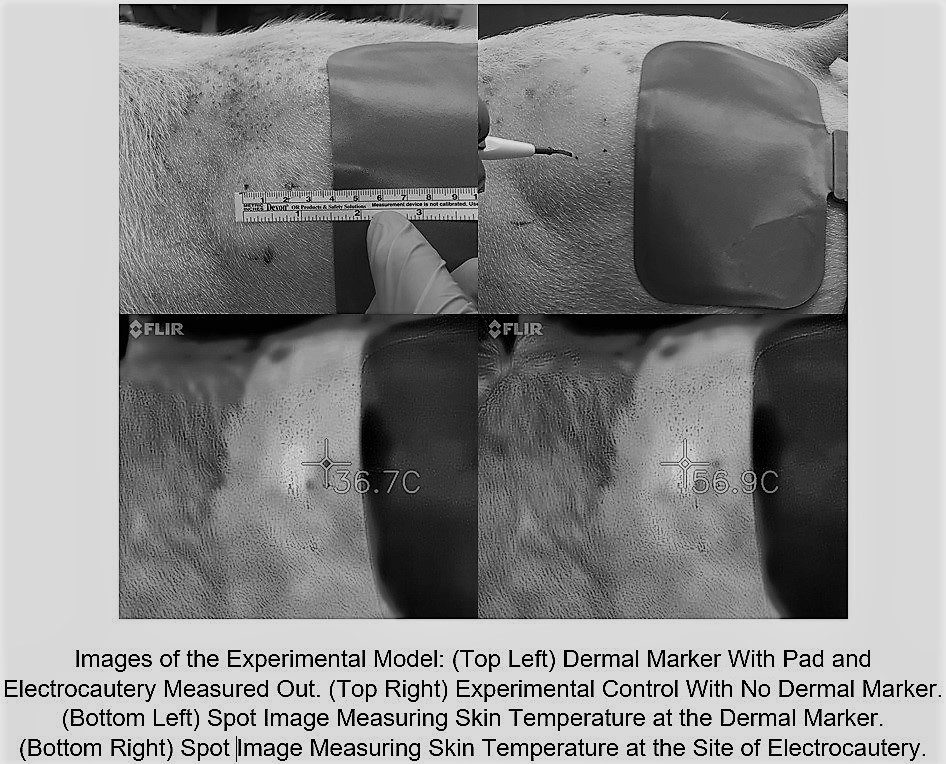
Methods: Stainless steel microdermal anchors (3 mm) were surgically implanted into 4 adult swine. Implants were placed into the bilateral flank and one of two randomized hindquarters. After 4 days to allow for initial healing and scar tissue formation, the bilateral flank implants were evaluated and excised for histologic examination. A Bovie electrocautery grounding pad was placed 2 cm caudal to the microdermal implant. Continuous electrocautery (coagulation/ 30 watts) for 30 seconds was applied to the skin at a point 2 cm cranial to the dermal implant. Surface skin temperature was recorded during electocautery using thermal imaging. Tissue damage was assessed by both gross examination and histologic evaluation of tissue immediately surrounding the excised microdermal implant. The same procedure was then performed to the contralateral non-implanted side as a sham control.
Results: Electrocoagulation for 30 continuous seconds raised the skin temperature around the electrocautery tip 49.9° F to an average of 148.7° F. Skin around the dermal implant only rose 3.24° F to an average of 101.7° F whereas the control skin without the dermal implant rose 3.65° F to 102.3° F (P=0.627). Skin temperatures at the dermal implant at 5 second intervals throughout the coagulation interval showed no statistical difference to those taken from the sham side at any time point. Histologic review of excised tissue samples showed no evidence of thermal injury.
Conclusion: Dermal implants appear to have no effect on skin temperature change during the use of electrocautery even when they are in close proximity to both the grounding pad and site of electocautery use. This suggests that microdermal implants may be safe and aggressive steps to ensure their removal before surgery are unnecessary.