A. M. White1, A. L. Halpern1, P. D. Koltz1, F. L. Grover1, C. D. Scott1, J. D. Mitchell1, M. R. Zamora1, R. A. Meguid1,2, L. J. Helmkamp2, D. A. Fullerton1, M. J. Weyant1 1University Of Colorado Denver,Cardiothoracic,Aurora, CO, USA 2The Adult and Child Consortium for Health Outcomes Research and Delivery Science,University Of Colorado,Aurora, CO, USA
Introduction: In this review, we evaluate patients with Interstitial Lung Disease (ILD) or Interstitial Pulmonary Fibrosis (IPF) as a single consortium of Pulmonary Fibrosis patients requiring transplantation. Our objective was to evaluate the effect of risk factors on survival in patients with Pulmonary Fibrosis who underwent lung transplantation using the United Network of Organ Sharing (UNOS) national database.
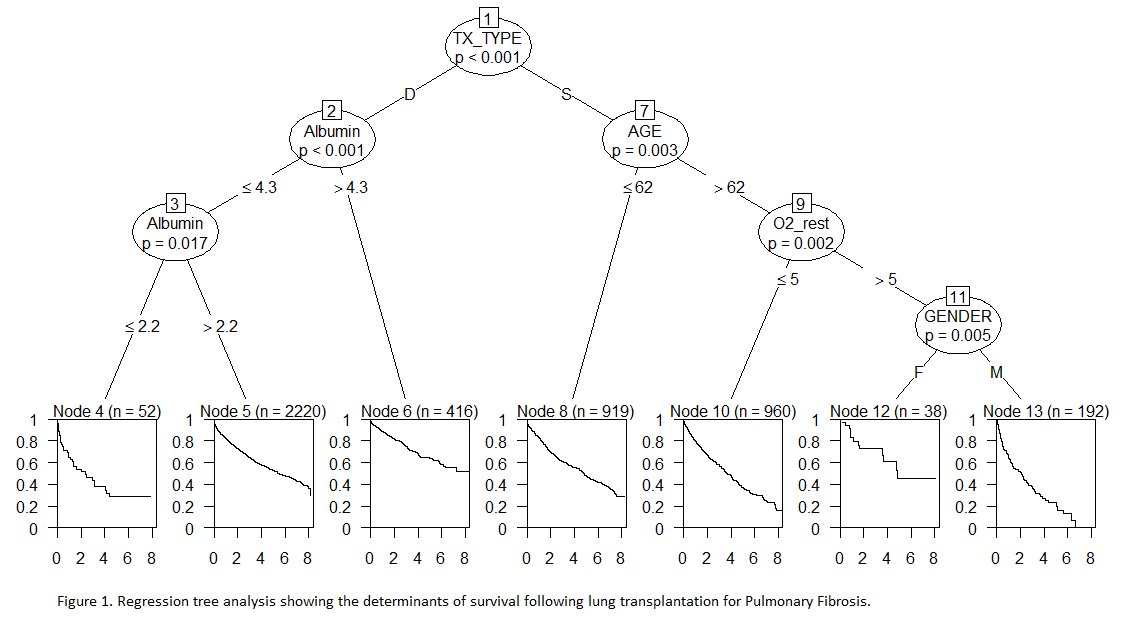
Methods: This is a retrospective cohort study using propensity matched multivariable regression and survival tree analysis models to examine multivariable associations between preoperative variables and mortality using data from 2005 to 2012 from the UNOS national database. Patients with a diagnosis of ILD, IPF, or subset of either who received a single or bilateral lung transplant were included in the study. Survival tree analysis was used to find important predictors of survival from a set of candidates including transplant type, serum albumin level, age, gender, pulmonary artery pressure, oxygen requirement at rest, BMI, six minute walk test, FEV1, and FVC percent of expected.
Results: The national database included 4,797 patients meeting criteria, with 2,109 undergoing SLTx and 2,688 undergoing BLTx. Overall, in a propensity matched analysis, BLTx had improved survival (HR 0.76, 95% CI 0.65, 0.87). In regression tree analysis showing the factors influencing survival, the first determinant is type of transplant, with bilateral lung transplant conferring improved survival (p-value <0.001). The second determinant of improved survival was high serum albumin pre-transplant, defined as > 4.3 g/dL (p-value < 0.001), with low serum albumin pre-transplant (defined as ≤ 2.2 g/dL) predictive of significantly decreased survival. Age ≤ 62 was also predictive of increased survival (p-value 0.003) as was lower oxygen requirement at rest and female gender.
Conclusion: In patients with Pulmonary Fibrosis receiving lung transplantation, the type of lung transplant received and serum albumin are important determinants of survival.