G. Yan1,4, K. T. Anderson1,4, J. K. Chica1,4, D. M. Ferguson1,4, G. E. Hatton1,4, J. C. Chapman3,5, E. M. Imseis3,6, A. Kawaguchi1,3,4, A. L. Speer1,3,4 1McGovern Medical School at UTHealth and Children’s Memorial Hermann Hospital,Department Of Pediatric Surgery,Houston, TEXAS, USA 3McGovern Medical School at UTHealth and Children’s Memorial Hermann Hospital,Short Bowel Syndrome Therapy And Rehabilitation (STAR) Team,Houston, TEXAS, USA 4McGovern Medical School at UTHealth and Children’s Memorial Hermann Hospital,Center For Surgical Trials And Evidence-based Practice (C-STEP),Houston, TEXAS, USA 5McGovern Medical School at UTHealth and Children’s Memorial Hermann Hospital,Department Of Pediatrics, Division Of Neonatology,Houston, TEXAS, USA 6McGovern Medical School at UTHealth and Children’s Memorial Hermann Hospital,Department Of Pediatrics, Division Of Gastroenterology,Houston, TEXAS, USA
Introduction:
Although achievement of enteral autonomy (EA) after pediatric intestinal failure (IF) is known to improve survival, the reported rates of and contributing factors to EA are highly variable in the literature. The aim of our study was to determine the incidence and predictors of EA in pediatric IF patients treated in a tertiary referral intestinal rehabilitation program.
Methods:
We conducted a single-center retrospective cohort study of pediatric (<18 years) IF patients (2013-2018). IF was defined as either a bowel resection or gastrointestinal motility disorder diagnosed at <1 year old requiring parenteral nutrition (PN) for ≥60 of 74 consecutive days. EA was defined as discontinuation of PN for >3 consecutive months with maintenance of growth variables. Demographics, clinical characteristics, and operative details were collected. Descriptive statistics, Wilcoxon-rank sum, chi2, and multiple logistic regression were used for analysis.
Results:
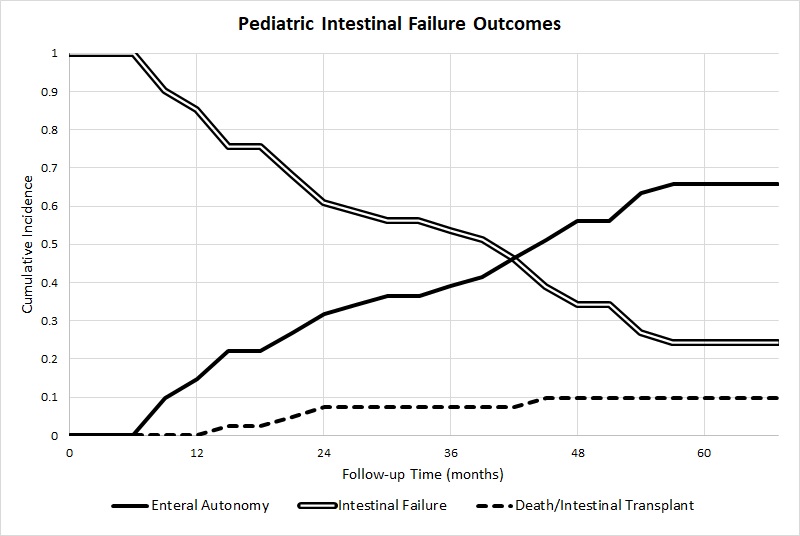
Forty-one patients met inclusion criteria. The majority were male (56%), other race (51%), non-Hispanic (58%), and Medicaid funded (90%). Median age at study inclusion was 85 days (IQR 76-102). Median gestational age was 30 weeks (IQR 25-34) and birth weight was 1170 grams (IQR 725-2140). The most common cause of IF was necrotizing enterocolitis (63%). EA was achieved in 27 patients (66%) at a median of 123 days (IQR 101-184). Of the 14 (34%) that did not achieve EA, 8 (20%) remained PN dependent, 4 (10%) died, and 2 (5%) weaned off PN but did not meet EA criteria. No patient underwent intestinal transplant (Figure). The median follow-up was 20 months (IQR 11-30). On univariate analysis, EA was associated with preserved ileocecal valves (ICV) (85 vs 36%, p=0.00), longer residual small bowel length (SBL) (60 vs 33 cm, p=0.01), and higher percent of expected SBL (42 vs 17%, p=0.01). Additionally, the following variables were identified as potential contributing factors to EA and used in our multiple logistic regression model: lower direct bilirubin (2.6 vs 3.9, p=0.14), lower aspartate aminotransferase to platelet ratio index (1.0 vs 1.7, p=0.08), decreased cholestasis (59 vs 86%, p=0.08) and increased restoration of intestinal continuity (91 vs 71%, p=0.14). Residual SBL and percent of expected SBL were omitted on multiple logistic regression analysis, due to incomplete data (n=21). Only a preserved ICV predicted achievement of EA (OR 5.65, CI 1.06-30.21).
Conclusion:
An EA rate of 66% was comparable to prior studies and was best predicted by ICV preservation. Efforts to preserve the ICV and SBL are paramount to the achievement of EA and, ultimately, to the survival of this vulnerable patient population.