R. Choudhury1, H. B. Moore1, K. Prins1, T. Nydam1 1University Of Colorado Denver,Transplant Surgery,Aurora, CO, USA
Introduction: Uncontrolled donation after cardiac death (uDCD) is a novel method to increase the supply of kidney allografts. As opposed to controlled DCD (cDCD), uDCD remains an underutilized practice in the United States. Its use in Europe, primarily Spain, has largely been restricted to out of hospital cardiac arrests (OHCA) with limited volumes of recoverably allografts. Given the high amount of unsuccessful resuscitations following trauma arrests (URTA) in the United States, various groups have suggested that this population should be included in a uDCD program. Estimates vary as to the number of potential kidney allografts which could be gained with this method. Furthermore, the impact on the rate of transplant and overall survival for a patient currently on the kidney transplant waitlist are unknown. The objective of this study was to estimate the impact of uDCD on the rate of transplant, chance of remaining on dialysis, and death for end stage renal disease (ESRD) patients on hemodialysis in the United States.
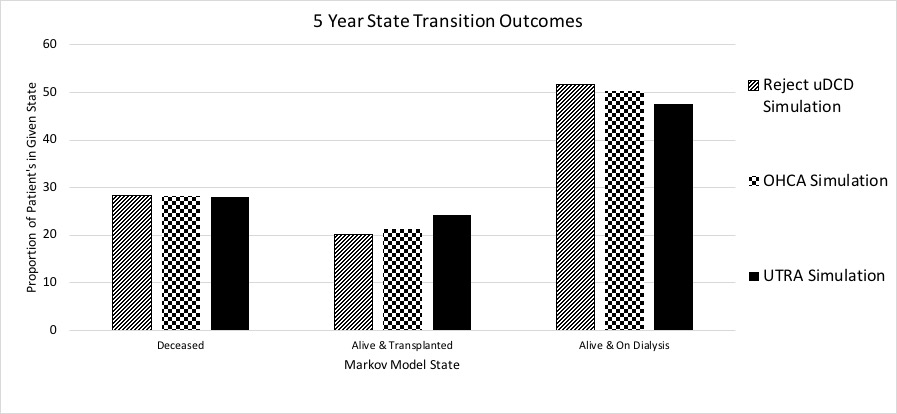
Methods: A decision analytic Markov state transition model was created using medical decision-making software (DATA 3.5, TreeAge Software, Inc., Williamstown, MA) in order to simulate three clinical scenarios for a group of 60,000 ESRD patients on hemodialysis who do not have access to a living donor (20,000 in each group). Three clinical scenarios were modeled: 1) Reject uDCD: Patients are on kidney transplant waitlist and will never accept a uDCD kidney, 2) OHCA simulation: On waitlist and will accept a OHCA uDCD kidney if available, whose availability is estimated from the high volume uDCD European center (Spain), and 3) UTRA simulation: On waitlist and will accept a URTA uDCD kidney if available, whose local availability is estimated from the experience of high volume level one trauma center in the United States (Denver Health). Markov model transition probability were calculated from the literature for “Reject uDCD” and OHCA simulations, and were derived from chart review of Denver Health Medical Center for the UTRA simulation.
Results: A UTRA uDCD program increases the rate of patients who are transplant at five years (24.3%, UTRA vs 21.3%, OHCA, vs 20.2%, Reject uDCD). Furthermore, patients who remain on dialysis are also reduced in the UTRA simulation. However, 5 year all-cause mortality is similar among groups (28.1%, 28.2%, 28.3%).
Conclusion: uDCD improves access to transplant for ESRD patients on the kidney transplant waitlist. However, all-cause mortality is similar for patients who reject uDCD suggesting that careful patient selection is required to match a potential uDCD kidney allograft to patients who would likely not be offered a transplant by any other means such that net utility may be gained.