M. T. Grant1, J. D. Vrecenak1 1Washington University,Pediatric Surgery,St. Louis, MO, USA
Introduction: In utero hematopoietic cell transplantation (IUHCT) is performed before the fetal immune system matures and thus requires neither myeloablation nor toxic immunosuppression, while allowing stable long-term engraftment of donor cells in a mixed chimeric state. Our laboratory has demonstrated that the fetal blood brain barrier is sufficiently permeable to allow for cellular trafficking of transplanted cells into the central nervous system (CNS) at a wide range of gestational timepoints in a murine model. Given the presence of donor-derived cells in this selective environment, we sought to investigate whether these cells were present in other highly regulated developmental niches such as the gonads. Furthermore, we sought to investigate whether mating IUHCT-derived chimeras would yield any detectable chimerism in offspring.
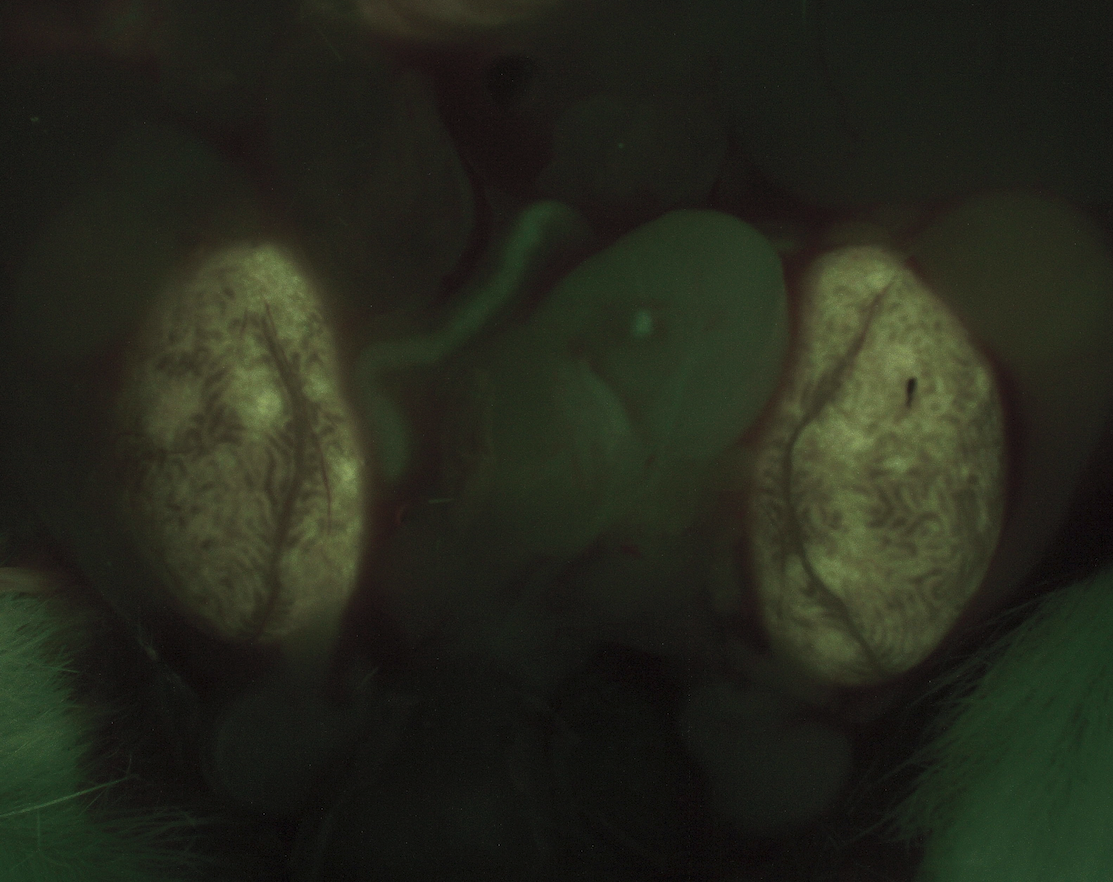
Methods: In preparation for IUHCT, BALB/c male mice were singly housed and paired with BALB/c females for a 24-hour period in order to achieve time-dated mating. Donor bone marrow (BM) was harvested from B6-GFP. Following ficoll separation, donor BM mononuclear cells were prepared for same-day injection. At gestational time points of 13 and 14 days, BALB/c dams found to be pregnant on exam underwent laparotomy and fetal intravenous injection of 20 x 106 GFP+ donor BM mononuclear cells per fetus via the vitelline vein. Resultant pups underwent peripheral blood chimerism analysis monthly through six months. Two male and two female pups found to have chimerism >20% were mated with untreated BALB/c mice of the opposite sex. The resultant offspring from those litters underwent chimerism analysis by flow cytometry at one month of age. Additionally, the first-generation chimeras underwent fluorescent stereomicroscopy of gonadal tissue at time of terminal harvest.
Results: As a result of IUHCT, 83% of the treated pups had chimerism levels greater than 20%. Both male and female chimeras yielded offspring of both sexes, none of which had any degree of chimerism in peripheral blood or bone marrow. Fluorescent stereomicroscopic examination of gonadal tissue from chimeras revealed low levels of fluorescence consistent with serosal engraftment, but no appreciable amount of fluorescence was present within the gonadal parenchyma.
Conclusion: Although donor-derived cells can engraft within tightly regulated developmental niches such as the CNS following IUHCT, the donor cells do not engraft within or alter the germline. Thus, the progeny of fetuses treated with IUHCT are not chimeric. This has significant clinical implications regarding reproductive planning for future patients treated with IUHCT, as their offspring could be affected by and/or carry the same genetic condition that necessitated treatment with IUHCT.