T. E. Habarth-Morales1,2, H. D. Davis1,3, A. J. Rios-Diaz1, E. J. Caterson4, R. B. Broach1, J. M. Serletti1, J. W. Swanson5 1University Of Pennsylvania, Division Of Plastic Surgery, Department Of Surgery, Philadelphia, PA, USA 2Thomas Jefferson University, Sidney Kimmel Medical College, Philadelphia, PA, USA 3Temple University, Lewis Katz School Of Medicine, Philadelpha, PA, USA 4Nemours Children’s Health, Division Of Plastic Surgery, Department Of Surgery, Wilmington, DELAWARE, USA 5Children’s Hospital Of Philadelphia, Division Of Plastic And Reconstructive Surgery, Philadelphia, PA, USA
Introduction: Late presentation craniosynostosis (LPC), loosely defined as presentation after one year of age, has been associated with more complex management and increased complications. We sought to describe the patient level factors associated with LPC using a national database.
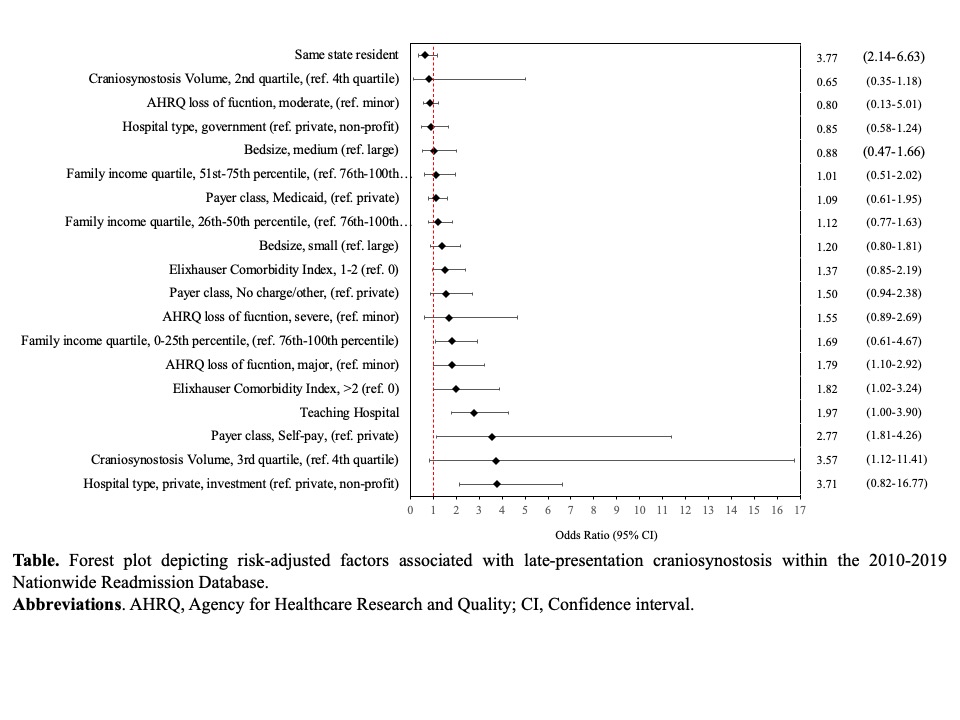
Methods: We identified patients diagnosed with craniosynostosis using the 2010-2019 Nationwide Readmissions Database (NRD). LPC cases were defined as those who underwent cranial vault remodeling (CVR) after 1 year of age. Multivariate logistic regression was used to identify patient and hospital level characteristics associated with LPC while generalized linear models were used to predict mean differences in length of stay and aggregate costs.
Results: A total of 10,830 cases of craniosynostosis who underwent CVR were identified. LPC patients made up 17% of these and tended to be from lower income families (56% vs 46%, 1st-50th percentile, P=0.044), had more comorbidities (3.4% vs 1.2%, >2, Elixhauser comorbidity index, P<0.001), and were more likely to be treated at teaching centers (98% vs 96%, P=0.010). Risk adjusted analyses showed that when controlling for confounders, LPC patients were more likely to be in the lowest income quartile (Odds Ratio [OR]: 1.79 [95% CI: 1.09-2.92, P=0.02]), more likely to receive treatment at privately owned investment hospitals (OR 3.71 [0.82-16.77], P<0.001), and were more likely to be self-pay (OR 2.77 [1.81-4.26], P=0.020) (FIGURE). LPC patients had a higher predicted mean total cost ($4,204 [$289-$8,119], P=0.035) compared to those who presented under a year of age while there was no difference in length of stay (0.23 days [-0.68-1.16], P=0.616). The total annual costs associated with treatment of LPC was USD $6,639,279 per year.
Conclusions: LPC patients are more likely to be from lower income families and incur higher costs during their hospitalizations compared with patients presenting prior to 1 year of age. Greater efforts should be undertaken to increase awareness of the increased costs and complications associated with LPC to families at greater risk to present late.