M. A. Sacks1, F. A. Velcek1 1SUNY Downstate Health Sciences University, Department Of Surgery, Brooklyn, NY, USA
Introduction:
Surgical residents are expected to obtain consent for complicated surgical procedures. Most residents have little training of informed consent prior to residency. Without understanding of the components of consent, the process can be challanging. We proposed a education and simulation workshop to address this issue. The purpose was to assess and improve the communication and consent process for pediatric general surgery cases by surgical residents.
Methods:
After internal review board(IRB) committee exemption for quality improvement project, a needs assessment was instituted to gather deficiencies in the communication process for pediatric surgery perioperative discussions. A grand rounds presentation was developed to address deficiencies in communication and highlight areas of improvement for the pediatric surgery consenting process. Pre/post-tests were developed to assess knowledge and growth after session. General surgery residents were assessed on comfort level for consenting families of patients for pediatric surgery procedures and confidence level in having difficult discussions with families for complex pediatric surgical cases. A grand rounds presentation served as the education session to explain definitions and present opportunities for simulation with feedback. After the session, residents rated their confidence in the above areas.
Results:
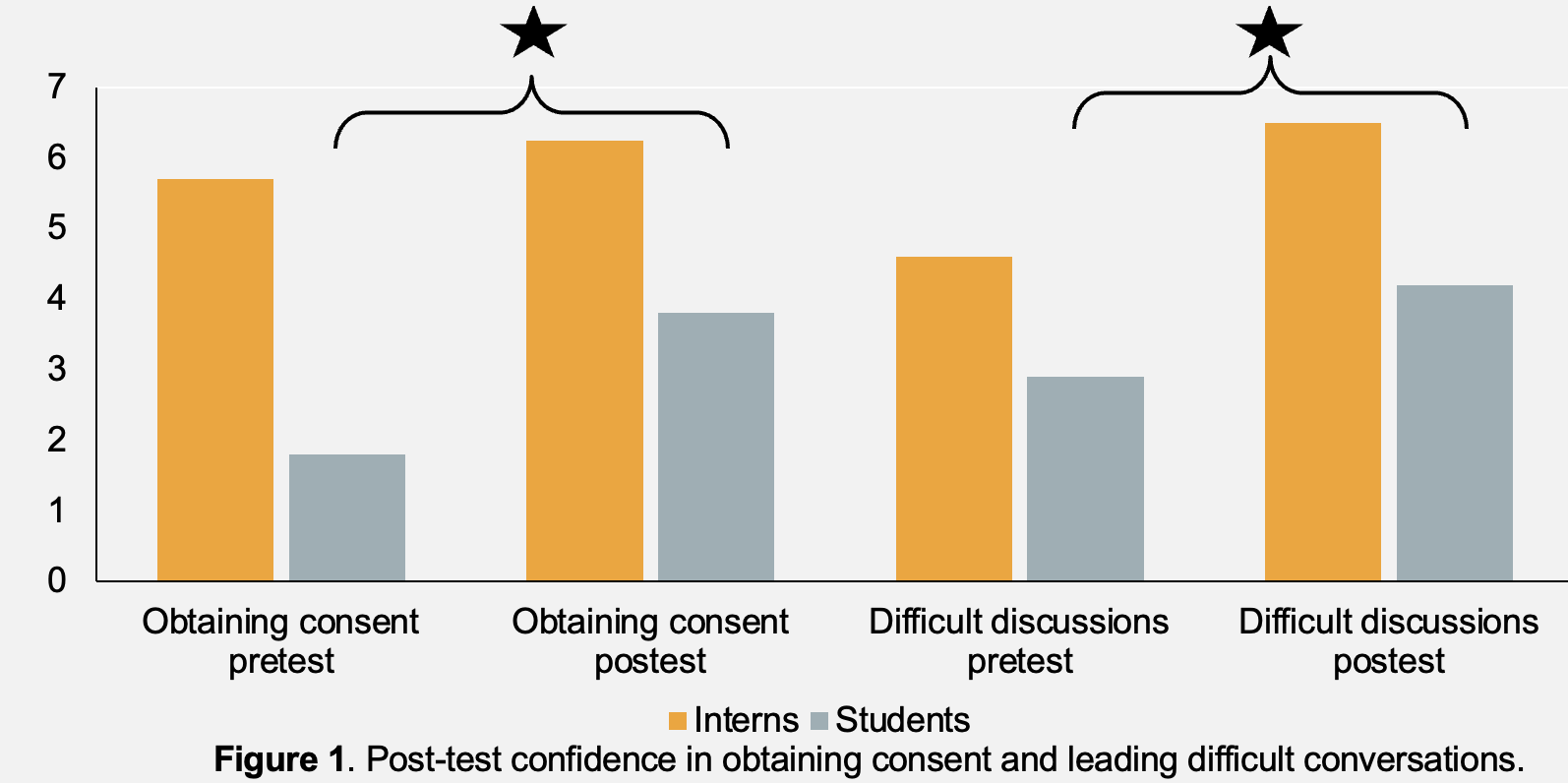
In this group of grand round attendees, following the session of education for consent components and having senior residents practice obtaining consent from faculty for procedures with open feedback, attendees found the session helpful. Where senior residents(PGY 4-5) gain was negligible, interns showed improvement in confidence having difficult discussion (4.6 -> 6.5) and medical students almost doubled their scores in confidence with obtaining consent (1.8 -> 3.8) and having difficult discussions (2.9 -> 4.2) after just observing the ground rounds session (Figure 1). Where communication errors cost time, money, productivity, and trust of the patient, this assessment and learning session attempted to close the gap for pediatric surgery cases.
Conclusion:
There is a need for discussions on consenting of pediatric patients with oversight. Residents lack education on who can consent and resources to improve the consenting process. A single short session is well-received by residents, which improved knowledge, boasted confidence, and provided and opportunity for quality improvement in the consenting process.