S. Prathibha1, S. Bejarano3, A. Z. Molina4, M. Zuniga2, J. Y. Hui1, J. Witt5, S. Marmor1, T. M. Tuttle1 1University Of Minnesota, Surgical Oncology/Surgery, Minneapolis, MN, USA 2One World Surgery, Tegucigalpa, FRANCISCO MORAZÁN, Honduras 3Liga Contra el Cancer, Clinical Oncology/Medicine, San Pedro Sula, CORTES, Honduras 4Hospital San Felipe, Clinical Oncology/Medicine, Tegucigalpa, FRANCISCO MORAZÁN, Honduras 5St. Luke’s Surgical Associates, Duluth, MN, USA
Introduction:
Breast cancer is the leading cause of cancer death in low and middle-income countries (LMIC). Delays to diagnosis and treatment are common in LMICs and result in advanced stage breast cancer and worse survival rates. Previous studies have demonstrated that lack of breast cancer information by primary providers in LMICs can lead to delays in diagnosis. Honduras, a LMIC, lacks robust research on breast cancer. The objective of this study is to survey baseline breast cancer knowledge among Honduran providers, present an educational conference on breast cancer and study possible improvements in knowledge.
Methods:
A one-day, in-person breast education conference directed towards primary care providers was held in Honduras on March 2023. Lectures, hand-on demonstrations, and tumor boards were included. A knowledge-assessment tool was created by breast cancer experts from Honduras and the United States and evaluated participant knowledge regarding screening, diagnosis, and treatment. Once informed consent was obtained, participants were asked to complete demographic and knowledge surveys before the start of the course. One month after the course, participants completed the survey again. Pre- and post-course scores were calculated, and descriptive statistics were used to analyze the scores.
Results:
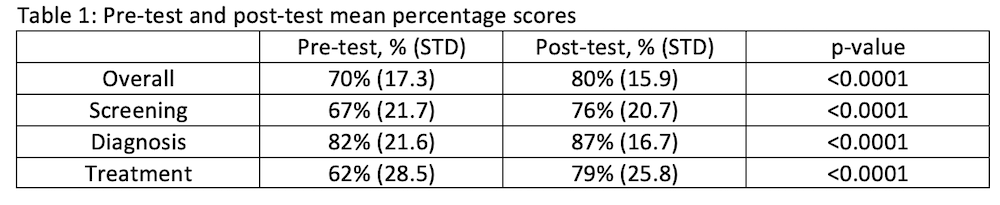
The initial survey received 86 responses and the 1 month post-course survey received 94 responses. 31% were physicians, 19% were nurses, 44% were other healthcare workers and 6% did not identify their field. Physician status, age, prior educational activities, number of years in practice, and number of breast cancer patient seen per month did not significantly impact initial baseline survey scores. Overall scores significantly improved from 70% at baseline to 80% at 1 month (p<0.0001). Similarly, scores evaluating screening (67% to 76%), diagnosis (82% to 87%), and treatment (62% to 79%) significantly increased from pre-course to 1 month post-course (Table 1).
Conclusion:
We found that the implementation of a one-day educational conference in Honduras resulted in significant improvement in knowledge scores regarding breast cancer screening, diagnosis, and treatment. Although further studies are required to understand whether this improvement is retained long term, this strategy may effective in reducing delays to breast cancer diagnosis and treatment in other LMICs.