M. MacRae1, M. Callaghan1, B. Tass3, T. McCallin3, E. Miyasaka2 2Rainbow Babies and Children’s Hospital, Pediatric Surgery, Cleveland, OH, USA 3Rainbow Babies and Children’s Hospital, Emergency Medicine, Cleveland, OH, USA 1Case Western Reserve University School Of Medicine, Cleveland, OH, USA
Introduction: Ultrasound (US) is a commonly employed method to aid in the diagnosis of acute appendicitis. However, US accuracy is dependent on the operator and appendix location, contributing to a high non-visualization rate. This study aims to describe patient characteristics that predict visualization of the appendix by US. We also aim to describe patient features that warrant further investigation for non-visualized appendices (NVA).
Methods: We performed a retrospective chart review of 726 pediatric patients who underwent 743 US for suspected appendicitis at a pediatric emergency department from November 2017 through December 2021. Imaging findings were characterized as positive, negative or NVA. Appendix location was classified as central, pelvic, retrocecal, anterior, or NVA. Patient age, sex, body mass index (BMI), pediatric appendicitis score (PAS), c-reactive protein (CRP) and diagnosis by surgical pathology were recorded. Descriptive statistics were obtained and comparisons between groups were done using chi-squared tests.
Results: Of the 743 ultrasounds in our study, 186 visualized the appendix while 557 were NVA. Appendix was more likely to be visualized in males (30.7% vs. 20.4%), with the highest visualization rate between ages 8-11 years in males (42.1%) and 10-12 years in females (35.5%). Visualization rate was lower after age 13 (18.3%) in both sexes. Visualization was inversely related to BMI, with 32.4% visualization for BMI <17.9, 26.9% for BMI 18–22.9, and 7.3% for BMI >23.
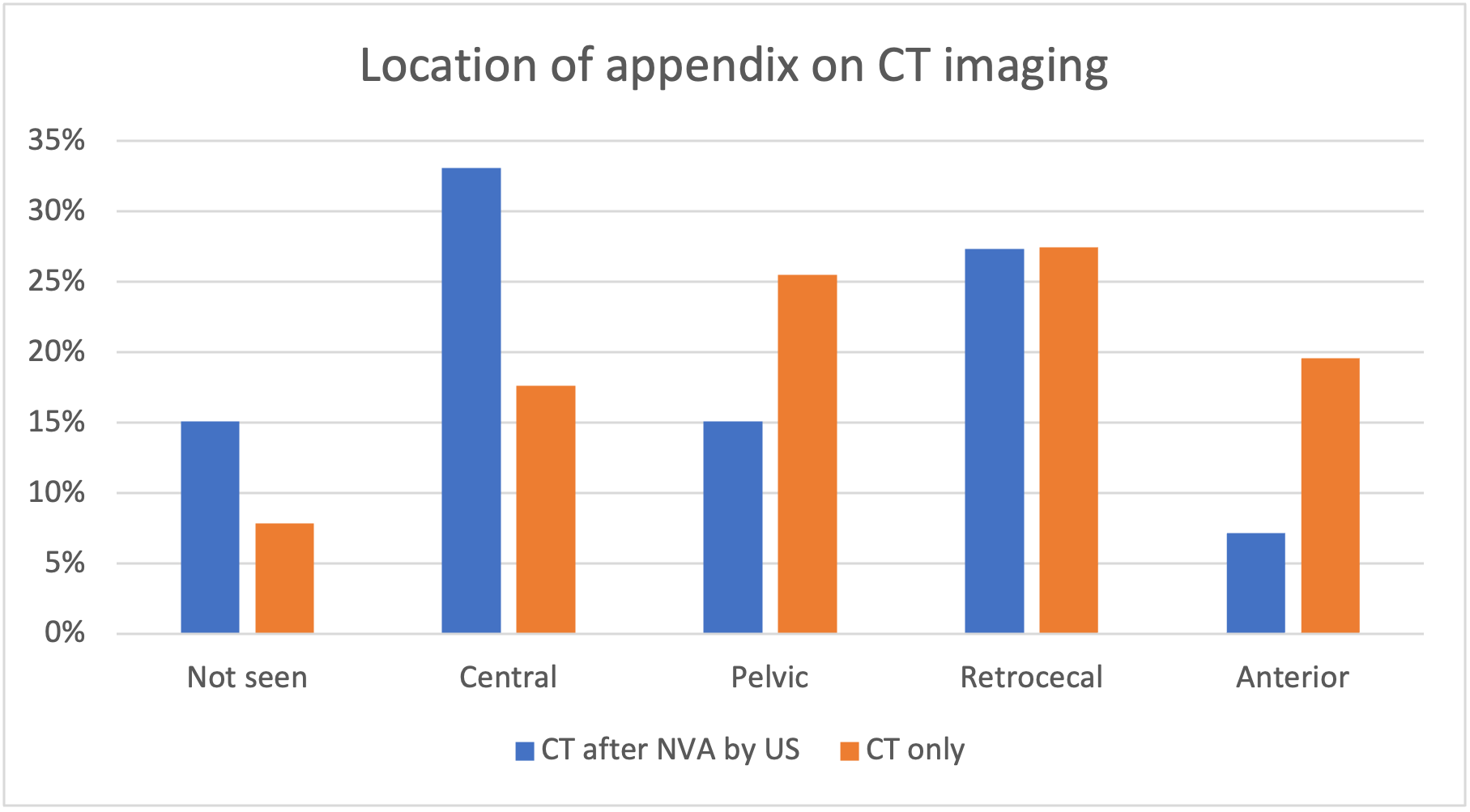
Distribution of appendix location by CT was significantly different between those who underwent CT after NVA by US (n=139) versus those who underwent primary CT scan (n=51). 60% of NVA were in the central or retrocecal positions (p=0.15, Figure 1).
Of NVA, 51 patients (9.2%) had acute appendicitis. These patients had higher average PAS (6.2 vs 4.4, p<.001), WBC count (15.5 vs 9.7, p<.001), neutrophil count (12.1 vs 6.0, p<.001), and CRP (7.6 vs 3.5, p<.001) compared to those without appendicitis. There was no correlation with sex, age, or BMI for NVA and the diagnosis of acute appendicitis.
Conclusion: US has highest visualization rate between the ages of 8-12, with better rates in patients with lower BMIs. Other diagnostic modalities including CT and observation should be more strongly considered in patients outside this category. Central and retrocecal locations of appendices were less likely to be visualized on US, suggesting that targeted re-scanning of this area may improve US visualization rates.