A. Vancheswaran2, A. Brenin1, C. Petrucci1, G. B. Rodriguez3, M. J. Ebanks3, M. G. Neuwirth2 1New York Medical College, Valhalla, NY, USA 2Westchester Medical Center, Department Of Surgery, Valhalla, NY, USA 3Westchester Medical Center, Department Of Surgery Clinical Research Unit, Valhalla, NY, USA
Introduction: Sentinel Lymph Node Biopsy (SLNB) is routinely recommended for the detection of nodal metastases in patients with malignant melanoma and T1b or greater primary tumors. Research has focused on the indication of SLNB based on T-stage and high-risk features; however, additional patient factors may significantly impact the prognostic value of SLNB. Increasing age has been associated with a higher incidence of melanoma death but a lower incidence of SLN metastasis. Studies suggest lymphatic drainage may become compromised with aging, undermining the utility of SLNB in predicting tumor spread in this population. This retrospective cohort study aims to better define the prognostic value of SLNB in patients as they age.
Methods: The National Cancer Database (NCDB) was used to identify individuals with clinical early stage melanoma to evaluate rates of SLN positivity. 58,571 patients with clinical node negative disease undergoing wide local excision and SLNB were included. Patients were categorized based on age, sex, clinical TNM stage, presence of ulceration, mitotic rate, and lymphovascular invasion (LVI). Joinpoint regression was used to analyze trends in SLN positivity across ages with further stratification according to T-stage.
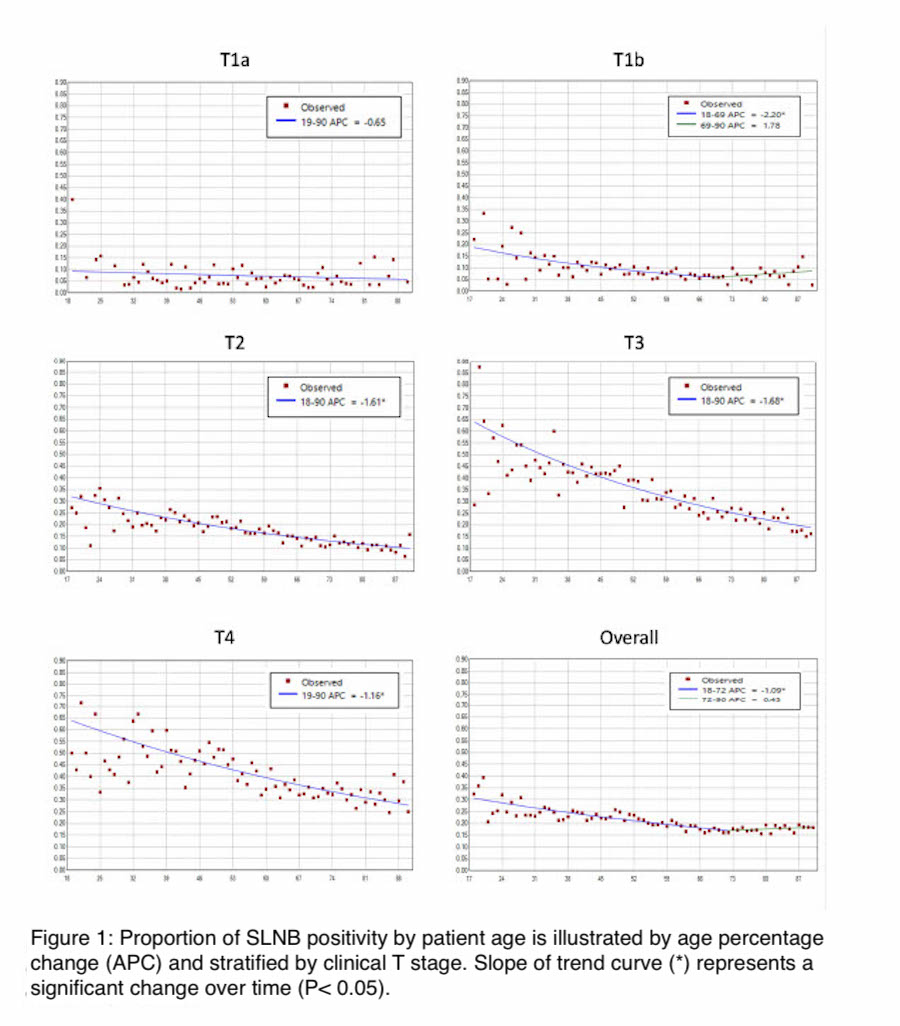
Results: Analysis of 58,571 patients revealed an overall SLNB positivity rate of 19.5%. SLNB positivity was significantly lower in patients over age 51 (p<0.001) and higher in advanced tumor stages (p<0.001). Joinpoint analysis (Fig. 1) for patients with clinical T1a-T4 disease demonstrated a statistically significant decrease in SLNB positivity rates until age 72 (Age percent change (APC) of -1.09%, p<0.05). When further stratified by clinical T stage, joinpoint regression showed a significant decrease in rate of SLNB positivity with age for clinical T stages T1b (APC -2.20 until age 69, p<0.05), T2 (APC -1.61, p<0.05), T3 (APC -1.68, p<0.05), and T4 (APC -1.16, p<0.05). Patients over 75 demonstrated significantly higher rates of ulceration, mitoses > 2/mm2, and LVI than patients in age groups <75 (p<0.001).
Conclusion: This study demonstrates that rate of SLNB positivity declines significantly with age across all T stages for which SLNB is routinely recommended in a generalizable sample derived from the NCDB. Despite this trend, patients over 75 consistently demonstrated more aggressive tumor features than younger patients. SLNB is not without morbidity, especially in frail populations. Based on these results, age should be taken into consideration independently of clinical tumor stage when considering patients for SLNB. Noninvasive staging modalities such as PET/CT and brain MRI may be considered for detecting spread of these higher risk tumors in an older population.