J. L. Williams2, I. A. Elliott1, A. H. Nguyen1, C. Matsumura1, R. Ghukasyan1, P. A. Toste1, J. R. Capri3, S. G. Patel1, L. Li1, N. Wu1, C. G. Radu3, T. R. Donahue1,3 1David Geffen School Of Medicine, University Of California At Los Angeles,Department Of Surgery,Los Angeles, CA, USA 2Harbor-UCLA Medical Center,Department Of Surgery,Torrance, CA, USA 3David Geffen School Of Medicine, University Of California At Los Angeles,Department Of Molecular And Medical Pharmacology,Los Angeles, CA, USA
Introduction: Pancreatic ductal adenocarcinoma (PDAC) is a highly lethal disease, with an overall survival of less than one year. Contributing to this poor prognosis is PDAC’s characteristically dense stroma, which is comprised predominantly of cancer-associated fibroblasts (CAFs). CAFs promote tumor growth, metastasis, and treatment resistance because when activated by environmental factors such as cancer cell (CC) exposure, hypoxia, and cytotoxic chemotherapy, they secrete protumorigenic cytokines, growth factors, and extracellular matrix components. However, elimination of CAFs also increases tumor growth and invasion. Therefore, rather than ablation, reprogramming of CAFs to an inactive or quiescent state is a potential PDAC treatment strategy. In this study, we aimed to determine the effect of PI3K/mTOR inhibition, a pathway known to be involved in fibroblast activation, on PDAC tumorigenicity.
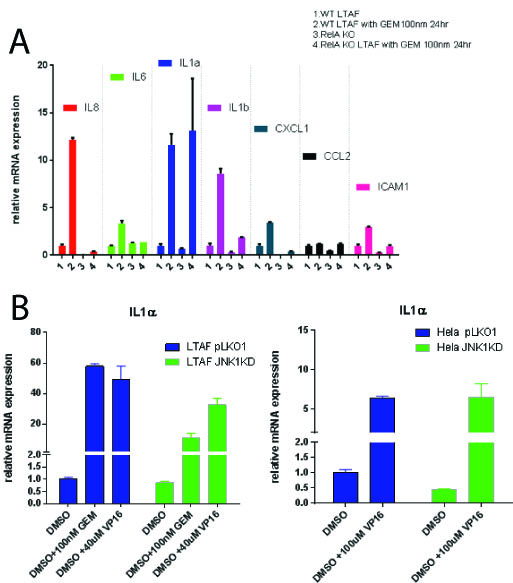
Methods: Immortalized CAFs were treated with NVP-BEZ235 (BEZ), a dual PI3K/mTOR inhibitor, and exposed to gemicitabine (GEM), hypoxia (1% O2), or PDAC CC conditioned media (CM) for 48 hours. After treatment, markers of CAF activation were determined via reverse transcription polymerase chain reaction (RT-PCR), Western blot, and mass spectrometry proteomics analysis of CAF CM. Additionally, PDAC CCs (Mia PaCa-2 and PANC-1) exposed to CM from treated CAFs were tested with in vitro viability, migration, and invasion assays. PDAC CCs were also co-injected with treated CAFs in vivo, and tumor size was assessed. A 3D co-culture model was used to assess the effect of BEZ treatment on CCs grown together with CAFs.
Results: After treatment with BEZ, gene expression of known markers of CAF activation, including alpha-smooth muscle actin (αSMA) and type I collagen, were decreased, even after exposure to activating stimuli. Similarly, αSMA protein levels were reduced in BEZ-treated CAFs. CM from BEZ-treated CAFs contained lower levels of extracellular matrix components, proinflammatory cytokines, and growth factors. CCs exposed to CM from BEZ-treated CAFs were less viable, migratory, and invasive in vitro. Pre-treatment of PDAC CAFs with BEZ restricted PDAC growth in our in vivo co-implantation model (Figure 1). In CC-CAF 3D co-culture, combination treatment of BEZ with GEM was more effective at suppressing CC growth than GEM treatment alone.
Conclusion: Inhibition of PI3K/mTOR decreases CAF activation, resulting in reduced PDAC CC tumorigenesis in vitro and in vivo. Additionally, combination treatment with BEZ, a dual PI3K/mTOR inhibitor, and GEM synergistically inhibits PDAC CC growth in the presence of CAFs. These data suggest that the addition of BEZ may improve the effectiveness of cytotoxic chemotherapy in PDAC.