Q. Dang1,2, S. Moradian1,2, J. Catino1, L. Zucker1, I. Puente1, F. Habib1, M. Bukur1 1Delray Medical Center,Department Of Trauma And Surgical Critical Care,Delray Beach, FL, USA 2Larkin Community Hospital,Department Of Surgery,Miami, FL, USA
Introduction: Traumatic Brain Injury (TBI) continues to be a leading cause of death and disability particularly in the elderly population. Age is generally considered to be a risk factor for adverse outcomes after TBI. We sought to examine the impact of age on outcomes in TBI patients who do not require neurosurgical operative intervention.
Methods: This was a retrospective review of all patients with survivable head injuries undergoing nonoperative management at a Level I trauma center from 2008-2013. Patients were stratified by age into young and elderly groups using the age of 40 as a reference group based upon the current Brain Trauma Foundation guidelines. Logistic regression was used to adjust for baseline differences in demographic and injury variables to determine the effect of age on outcomes. The primary outcomes were in-hospital mortality, worsening discharge GCS, and discharge disposition.
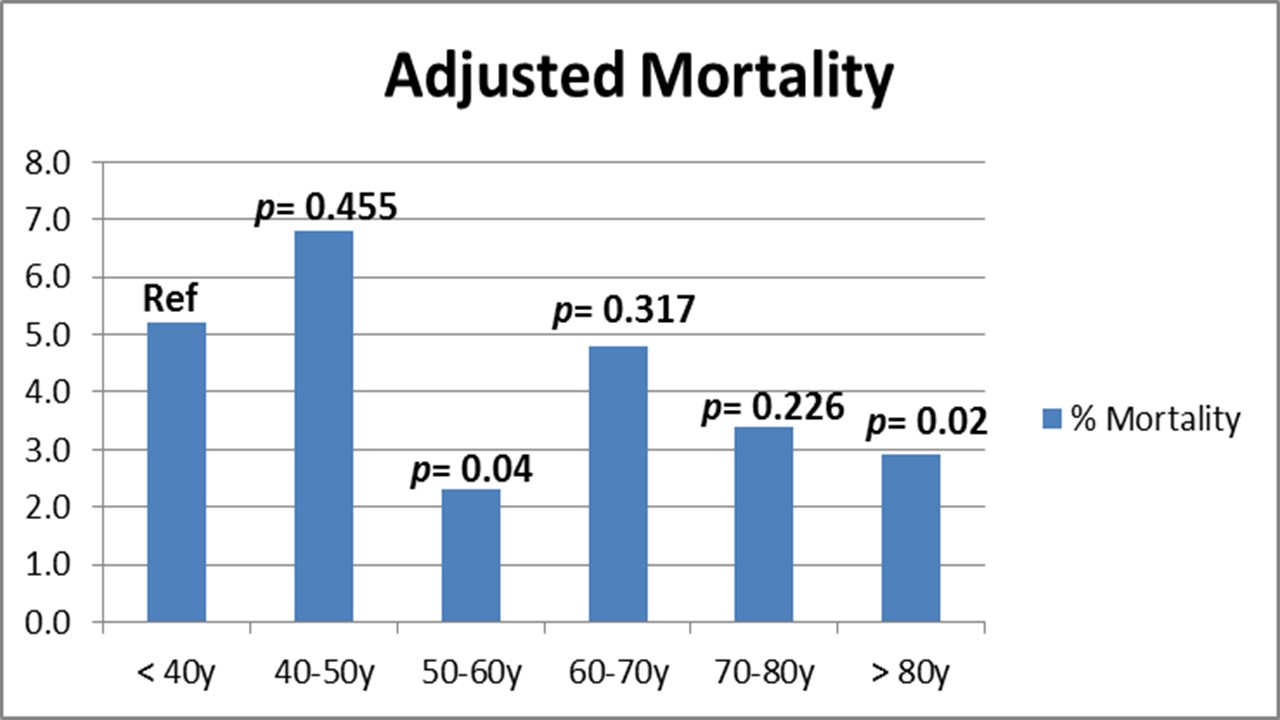
Results: 1,869 patients met inclusion criteria with 77% of patients being older than 40 years. Elderly patients were more likely to be victims of falls and presented with a higher GCS despite having a higher Head AIS. Immediate need for non-intracranial operative intervention was greater in younger patients. After adjusting for differences in characteristics, there was no significant difference in overall mortality (Elderly 3.6% vs. young 5%, p=0.209) or worsening discharge GCS (14% vs. 11%, p=0.926). However, younger patients were more likely to be discharged to a rehabilitation facility or home (91% vs. 70%, AOR=2.4, p=0.001). Stratification of mortality by decade revealed similar results, with adjusted mortality being lower in the sixth and ninth decades of life (Figure).
Conclusion: Survival of patients sustaining TBI not requiring neurosurgical operative intervention may not be age dependent. However, age is associated with a less favorable discharge disposition that is independent of discharge GCS.