A. J. Jacobs2, J. Fishbein3, C. Fein Levy4, R. D. Glick1 1North Shore University And Long Island Jewish Medical Center,CCMC, Division Of Pediatric Surgery,Manhasset, NY, USA 2Hofstra North Shore-LIJ School Of Medicine,Hempstead, NY, USA 3Feinstein Institute For Medical Research,Biostatistics Unit,Manhasset, NY, USA 4North Shore University And Long Island Jewish Medical Center,CCMC, Department Of Pediatric Hematology/Oncology,Manhasset, NY, USA
Introduction:
The globally low incidence of pediatric chest wall Ewing sarcoma (CWES) has limited prior studies of this disease to mostly small, single institution reviews. Our objective was to assess incidence, demographics, treatment patterns, and long-term survival of this disease through a population based analysis.
Methods:
The Surveillance, Epidemiology, and End Results (SEER) database was used to identify patients aged 0-21 diagnosed with CWES from 1973-2011. Patients were grouped by decade to assess changes in treatment patterns and outcomes. The effects of clinical, demographic, and treatment variables on overall survival were assessed by the computation of Kaplan-Meier curves and the log-rank test, with Cox proportional hazard regression used for multivariate analysis.
Results:
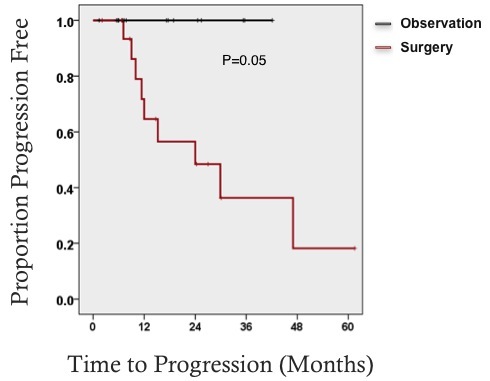
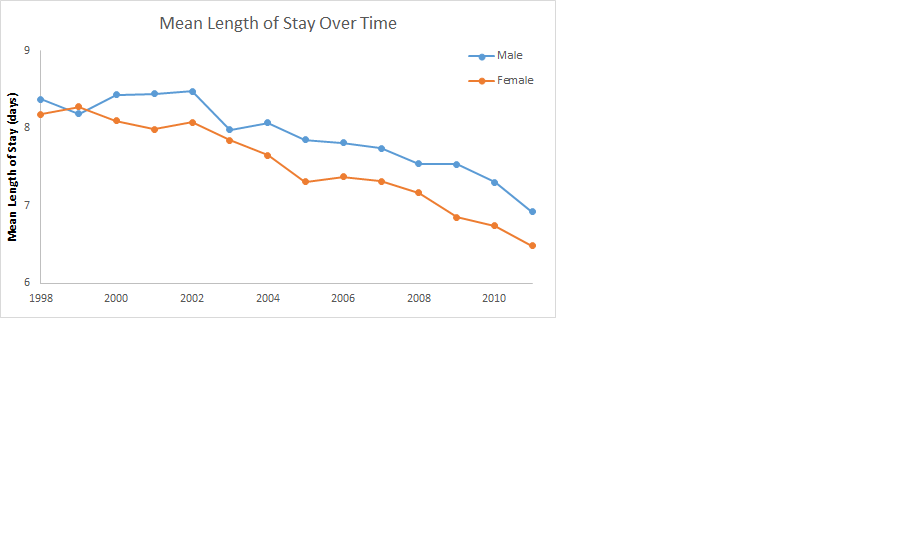
A total of 193 pediatric patients with histologically-confirmed CWES were identified. The disease was more common in males (60.6%), whites (92.2%), and 11-17 year-olds (48.7%). It was metastatic at presentation in 36.8% of patients. When grouped approximately by decade, 10-year overall survival improved progressively from 38.2% in 1973-1979 to 65.4% in 2000-2011 (p=0.033). The use of radiation decreased from 84.2% in the earliest time period to 40.0% in the most recent, while the proportion of patients receiving surgery increased from 75.0% to 84.9%. When controlling for covariates on multivariate analysis, male patients were found to have a higher mortality than female patients (HR: 2.4; CI: 1.4, 4.4; p=0.0028).
Conclusion:
This population-based analysis of CWES demonstrated an impressive trend of improving overall survival, with increasing use of surgery and decreasing use of radiation therapy. As has been previously noted for Ewing sarcoma in general, our study demonstrated a gender difference in survival of CWES, with girls having a better prognosis.