M. A. Mann1, M. Grimes1, M. L. Blute1, K. Zorn1, T. M. Downs1, S. L. Best1, F. Shi1, D. F. Jarrard1, S. Y. Nakada1, E. Abel1 1University Of Wisconsin,Urology,Madison, WI, USA
Introduction: Extreme or class 3 obesity (BMI ≥ 40) may be associated with increased morbidity following surgery. The objective of this study was to evaluate if patients with extreme obesity had worse perioperative outcomes following renal surgery.
Methods: Comprehensive medical records were reviewed for all patients treated with partial nephrectomy, radical nephrectomy or nephroureterectomy at our institution from 2000-2014. Complications occurring within 90 days were recorded and classified according to the Clavien-Dindo system. Univariable and multivariable models were used to evaluate the association of obesity with major complications (≥Clavien 3a), surgical site infections (SSI), blood transfusion (BT) rates and readmission rates.
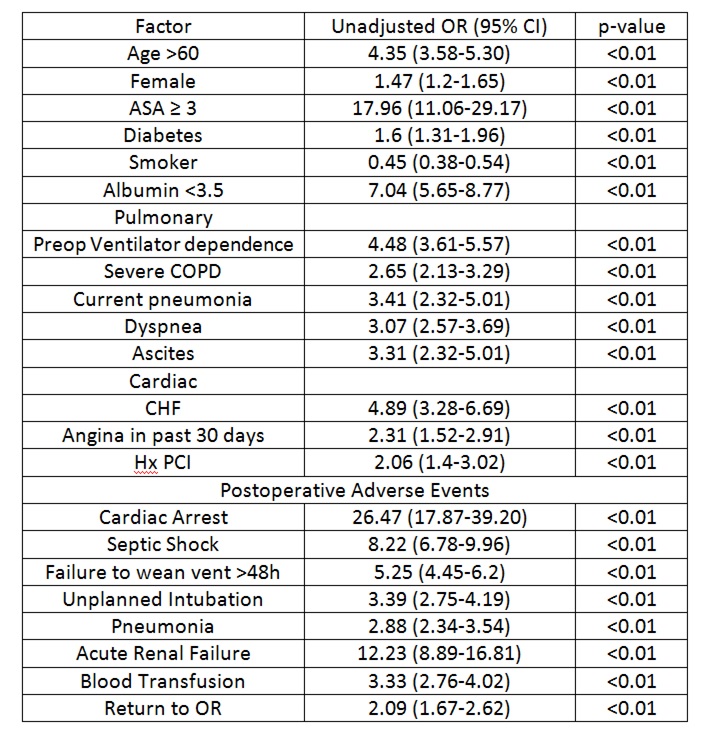
Results: A total of 1109 patients were evaluated including 114 (10.3%) patients with BMI ≥40. Perioperative complications were identified in 279 (25.5%) patients including major complications in 80 (7.3%). Patients with BMI ≥40 were not at increased risk for major complications (p=0.2). Independent predictors of major complications included Charlson Comorbidity Index and surgical approach (open vs. minimally invasive).
A total of 217 (19.6%) patients received BT during the initial hospitalization following surgery. BMI ≥40 was not associated with increased risk of BT (p=0.9) SSI were observed in 60 (5.5%) patients. Patients with BMI ≥40 had an increased risk of SSI, OR 2.3 (95% CI 1.2-4.5).
A total of 59 patients (5.4%) were readmitted to the hospital with 30 days following surgery. BMI ≥40 was not associated with increased risk of readmission (p=0.4)
Conclusion: Extreme obesity is associated with increased risk of wound complications but not a higher risk of major complications, BT, or hospital readmission following renal surgery. When feasible, minimally invasive surgery may be associated with lower major complication rates.