A. H. Othman1, A. Morales-Gonzalez1, M. Zuber2, V. Olivas1 1Texas Tech University Health Sciences Center,Surgery,El Paso, TX, USA 2Texas Tech University Health Sciences Center,OB GYN,El Paso, TX, USA
Introduction: To identify predictors of anastomotic leak (AL) in patients undergoing partial or total colorectal resection and anastomosis.
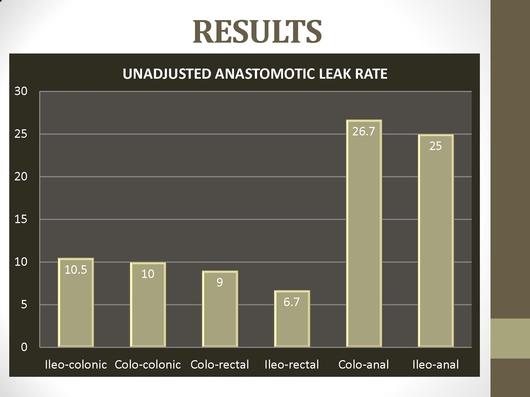
Methods: A retrospective cohort study was conducted at a single urban academic hospital in El Paso, Texas. Adults who underwent a partial or total colorectal resection with an ileo-colonic, colo-colonic, colo-rectal, ileo-rectal, colo-anal or ileo-anal anastomosis, between 2002 and 2012 were eligible for inclusion in the sample. Our cohort was composed of 537 procedures performed on 510 patients. Logistic regression using backward elimination was used to identify predictors of an AL. Adjusted odds ratios (OR) for AL, 95% confidence intervals (CI), and P values were calculated assuming statistical independence.
Results: The overall AL rate was 10.4%. Of the 510 patients, 88% were of Hispanic ethnicity. 37.5% of the patients who experienced AL and 25.0% of those who did not, were diabetic (P=0.04). The final regression equation contained two predictors: diabetic status and the type of resection. Diabetics were more likely to experience AL: adjusted OR=1.97 (95% CI: 1.07-3.63, P=0.03). Patients whose type of resection was colo-anal vs. ileo-colonic were more likely to develop an AL: adjusted OR=4.85, 95% CI: 1.33-17.69, P=0.02).
Conclusion: Diabetes and colo-anal anastomosis are associated with a higher risk of AL and should be considered and evaluated in the pre-operative surgical planning.