L. R. Putnam1,2, T. G. Ostovar-Kermani1,2, K. T. Anderson1,2, D. H. Pham1,2, M. T. Austin1,2, A. L. Kawaguchi1,2, L. S. Kao3, K. P. Lally1,2, K. Tsao1,2 1University Of Texas Health Science Center At Houston,Pediatric Surgery,Houston, TX, USA 2Children’s Memorial Hermann Hospital,Pediatric Surgery,Houston, TX, USA 3University Of Texas Health Science Center At Houston,General Surgery,Houston, TX, USA
Introduction: Standardized clinical care pathways for pediatric appendicitis are widely endorsed among children’s hospitals, yet their influence on patient outcomes is unknown. We aimed to determine the impact of a clinical care pathway for appendicitis, implemented at our children’s hospital in 2011, on length of stay, readmissions, and complications.
Methods: Pre-pathway data were compared to data from prospectively-monitored care pathways for all pediatric patients (<18 years) who underwent an appendectomy for acute appendicitis between June 2009 – December 2010 (pre-pathway) and January 2011 – May 2015 (pathway). Separate pathways were implemented for simple and complicated (gangrenous or perforated) appendicitis patients. Clinical outcomes including surgical site infections (SSI), initial and aggregate 30-day hospital length of stay (LOS), and readmissions within 30 postoperative days were recorded. Chi-squared, Student’s t-tests, Mann-Whitney U tests, and multivariate regression were performed; p-values <0.05 were considered significant.
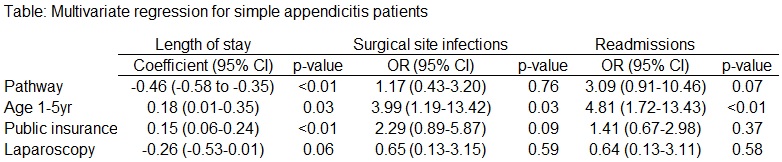
Results: 2151 patients (pre-pathway: 582, pathway: 1569) underwent appendectomy for acute appendicitis from June 2009 – May 2015. Mean age of pre-pathway vs pathway patients was 9.9 ± 3.7 vs 10.4 ±3.8 (p=0.01). Gender, race/ethnicity, and insurance status were similar between groups (all p>0.05). Simple appendicitis pathway patients experienced decreased initial LOS (1.4 vs 0.9 days, p=0.03) and aggregate 30-day LOS with no difference in SSI, but increased readmissions (1.3% vs 3.4%, p<0.05). There were no significant differences in outcomes for complicated appendicitis pathway patients. On multivariate regression analysis of patients with simple appendicitis, the pathway predicted shorter LOS; younger age and public insurance predicted increased LOS and SSI (Table). For complicated appendicitis patients, laparoscopic appendectomy was associated with decreased LOS; there were no significant predictors of SSI or readmissions.
Conclusion:Clinical pathways do not appear to substantially improve outcomes in pediatric appendicitis. Within our institution, the clinical pathway for simple appendicitis patients was associated with decreased initial and aggregate 30-day LOS, but increased readmissions, whereas the complicated appendicitis pathway was not associated with any improvements. Further efforts should target decreasing readmissions for simple appendicitis patients and determining the impact of pathways on hospital resource utilization. Although there are many benefits to protocolized care, the true efficacy of increasing standardization may lie in process improvement and not directly related to patient outcomes.