R. S. Jawa1, J. E. McCormack1, E. C. Huang1, M. J. Shapiro1, J. A. Vosswinkel1 1Stony Brook University Medical Center,Stony Brook, NY, USA
Introduction: Extremity compartment syndrome is a recognized complication of blunt trauma, especially with underlying fractures, where rates in excess of 10% have been reported. We sought to evaluate the prevalence and outcomes of extremity compartment syndrome at a suburban regional trauma center.
Methods: The trauma registry was retrospectively reviewed for all admitted adult (age>18) blunt trauma patients admitted from 2010 to 2014. Deaths in the emergency department and burns were excluded.
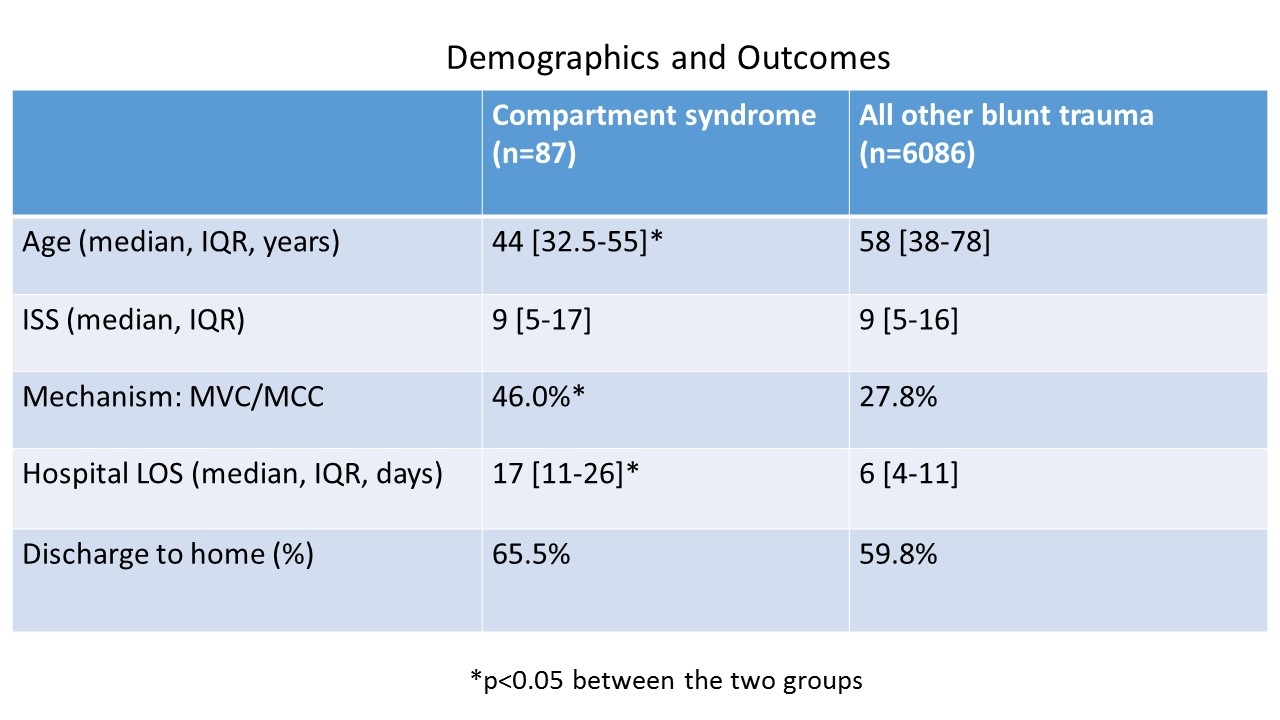
Results: During this time period, there 6173 adult blunt trauma admissions, of which 87 developed extremity compartment syndrome and were further evaluated (table). Their median age was 44 years [IQR 32.5-55] and the vast majority (90.8%) were male. While 76.9% had a National Trauma Data Standard (NTDS) defined comorbidity, 36.8% had ≥ 2 NTDS defined comorbidities. The most common mechanism was MVC (46.0%) followed by fall (23.0%). The median ISS was 9 [IQR 5-17]. The primary severe injury (AIS >3) locations in order of frequency were extremity (63.2%), followed by chest (16.1%), and abdomen (12.6%). Further 96.5% of these patients underwent major surgery, with the overwhelming majority being major orthopedic surgery (96.5%), followed by major abdominal surgery (8.0%). The median hospital LOS was 17 days [IQR 11-26], 34.5% required ICU admission with a median ICU LOS of 6 days [IQR 3.4-19.5], and 34.5% required mechanical ventilation. Further 44.8% had a complication. While 65.5% of admissions were discharged to home, 32.2% did require acute rehabilitation, and 2.3% died during hospitalization. This mortality rate was not significantly different from the rate in other blunt trauma patients (4.0%).
The vast majority (82.7%) of patients had lower extremity compartment syndrome. The most commonly injured bone associated with a compartment syndrome was the tibia (61.5%, n=48); in these 48 patients, it was associated with fibula fractures in 32 patients and with acetabular or other lower extremity fractures in 18 patients. Finally, 10.3% of patients did not have any fracture: 3 had contusions, 1 contusion with venous injury, 1 contusion with arterial injury, 1 sciatic nerve injury, and 3 crush injuries.
Conclusions: The prevalence of extremity compartment syndrome was quite low during this time period at 1.4%. Compartment syndrome most often (82.7%) occurred in the lower extremity, with the tibia being the most frequent fractured bone. However, 37.8% had minor extremity injuries (AIS ≤ 2); 10.3% of patients without a fracture had compartment syndrome. Vigilance is warranted in evaluating the compartments of patients with and without severe extremity injuries, even in the absence of underlying fracture.