S. E. Covey1, L. R. Putnam1,2, K. T. Anderson1,2, K. P. Lally1,2, K. Tsao1,2 2Children’s Memorial Hermann Hospital,Pediatric Surgery,Houston, TX, USA 1University Of Texas Health Science Center At Houston,Pediatric Surgery,Houston, TX, USA
Introduction: Intestinal malrotation can lead to midgut volvulus resulting in sepsis, short bowel syndrome, and death. Treatment includes the Ladd procedure to correct intestinal malrotation for symptomatic patients. However, debate remains regarding the timing of the procedure for asymptomatic infants with known malrotation. We hypothesized that the benefits of prophylactic Ladd procedure outweigh the risks of post-symptomatic repair.
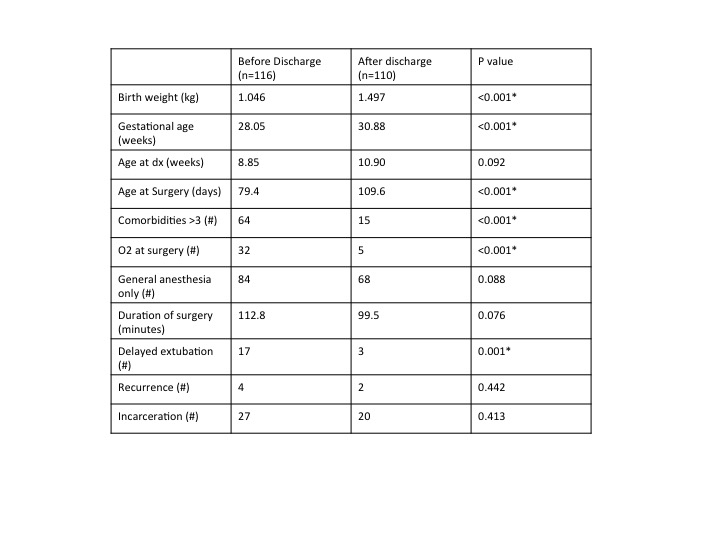
Methods: A retrospective chart review of pediatric patients undergoing the Ladd procedure was performed. Prophylactic Ladd procedures were identified as those that occurred prior to any malrotation-related symptoms (i.e. abdominal pain, distention, nausea, emesis, constipation, or feeding intolerance). Results were analyzed with Mann-Whitney U and chi-squared tests.
Results: From 2011-2014, 42 patients (prophylactic=19, post-symptomatic=23) underwent the Ladd procedure for intestinal malrotation. The median (interquartile range) age of patients was 9.6 (3.9-18) months and 18 (2.4-52) months for prophylactic and post-symptomatic patients, respectively (p=0.38). In patients who underwent post-symptomatic Ladd procedures, 9 (39%) were found to have volvulus and 1 (4.3%) had bowel necrosis at time of surgery. No prophylactic Ladd procedure patients required reoperation while 6 (26%) post-symptomatic patients required reoperation for gastrointestinal-related complications (p=0.02). Prophylactic versus post-symptomatic Ladd procedure patients required a median (interquartile range) of 5.0 (3.3-6.8) days vs 7.4 (5.0-11) days to tolerate full enteral feeds (p=0.11) and 8.0 (6.1-11) days vs 11 (7.5-32) days until discharge (p=0.09). There was one respiratory-related death in each group.
Conclusion: Although the post-symptomatic group represents sicker children, the postoperative complications appear to be higher. For infants with known malrotation, prophylactic operations may be beneficial and should be considered. A larger, prospective study comparing prophylactic Ladd procedures to observation is needed to demonstrate its comparative effectiveness and generalizability.