X. D. Pham1, V. F. Sullins1, D. Y. Kim1, B. Range3, A. Kaji2, C. DeVirgilio1, S. L. Lee1 1Harbor-UCLA Medical Center,General Surgery,Torrance, CA, USA 2Harbor-UCLA Medical Center,Emergency Medicine,Torrance, CA, USA 3University Of California – Los Angeles,Los Angeles, CA, USA
Introduction: The ability to predict whether a child has complicated appendicitis at initial presentation may influence clinical management. However, it is controversial whether complicated appendicitis is associated with prehospital factors (age, symptom duration, serum sodium, and WBC count) or in-hospital factors (time from admission to appendectomy). We investigate which of these factors are associated with predicting complicated appendicitis.
Methods: A retrospective review of all pediatric patients (≤12 years) with appendicitis treated with appendectomy between 2000-2013 was performed. The main outcome measure was intraoperative confirmation of gangrenous or perforated appendicitis. A multivariable analysis was performed and the main predictors of interest were age, symptom duration >24 hours, leukocytosis (WBC count >12 103/ml), hyponatremia (sodium <135 mEq/L), and time from admission to appendectomy.
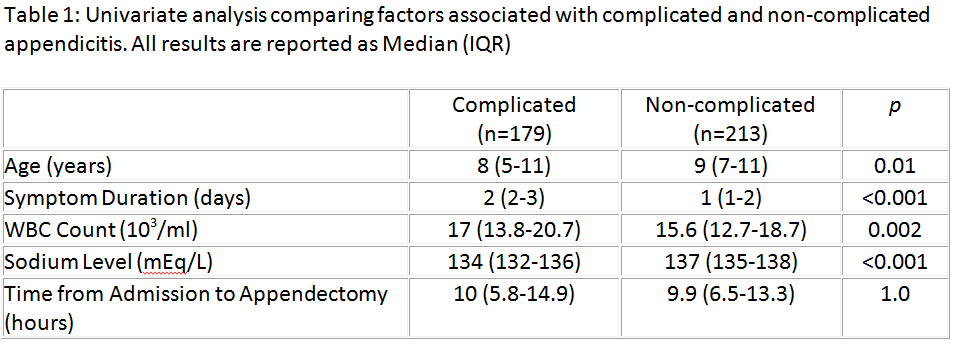
Results: Of 392 patients, 179 (46%) had complicated appendicitis at the time of operation. Results of univariate analysis are listed in Table 1. Predictors of complicated appendicitis on multivariable analysis included symptom duration >24 hours (OR=5.1, 95% CI=3.2-8.2, p<0.001), hyponatremia (OR=3.2, 95% CI=2-5.1, p<0.001), age <5 years (OR=2.7, 95% CI=1.3-5.4, p=0.007), and leukocytosis (OR=1.9, 95%CI=1-3.4, p=0.04). Increased time from admission to appendectomy was not a predictor of complicated appendicitis (OR=0.75, 95% CI=0.5-1.1, p=0.2).
Conclusions: Complicated appendicitis is a prehospital occurrence. Hyponatremia is a novel marker associated with complicated appendicitis and may be more predictive than WBC count or age. Delaying appendectomy does not increase the risk of complicated appendicitis. This information may help guide resource/personnel allocation, timing of appendectomy, and decision for non-operative management of appendicitis in children.