A. L. Hoffman1, W. J. Grant1, M. F. McCormick1, E. E. Jezewski1, A. N. Langnas1 1University Of Nebraska Medical Center, Surgery, Omaha, NE, USA
Introduction: Recent studies have examined gender differences in letters of recommendation for men and women in academic positions, research grant applications, and residency programs. No published study has explored such gender differences in applications to surgical subspecialty fellowships.
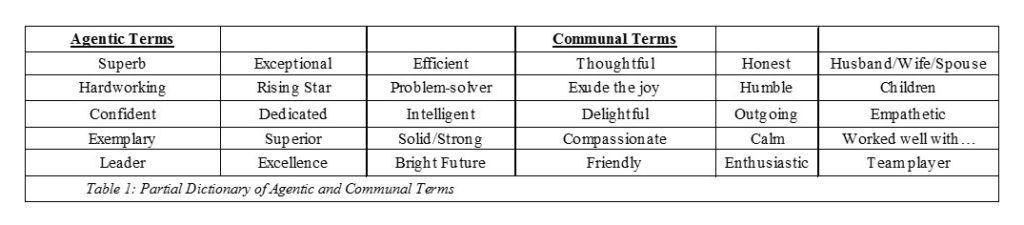
Methods: We conducted a retrospective review of 317 letters of recommendation to a transplant surgery fellowship written for residents finishing United States general surgery residency programs. We created a dictionary of communal and agentic terms (Table 1) and determined whether there were differences in the terms, characteristics, and length of the letters based on applicant’s gender as well as the academic rank and gender of the author.
Results: Of the 317 reviewed letters, 235 were letters of recommendation written for male applicants. Male surgeons wrote 91.76% of letters written for female applicants and 93.2% of letters written for male applicants. Full professors wrote 58.7% of the letters, associate professors wrote 19.2% and assistant professors wrote 21.13%. Male applicant letters were significantly more likely to contain agentic terms than female applicant letters (p=0.00086). Additionally, male applicant letters were significantly more likely to contain the term “future leader” than female letters (p=0.047). Letters containing the term “future leader” were more agentic (p=< 0.0001) and less communal (p=0.047) than letters that did not contain this term. Letters written by full professors, division chiefs, and program directors were significantly more likely to describe female applicants using communal terms like compassionate, calm and delightful (p=0.0301, p=0.036,p= 0.036 respectively). In letters written by assistant professors, female letters had significantly more references to the applicants family (p= 0.036) and were longer (p=0.00554) than male letters. We identified terms only found in male letters “no doubt will become extremely successful”, “is a great rarity”, “indestructible machine”, and “unlimited power”, as well as terms only found in female letters “successfully balancing work and family”, “blossomed”, “achieved without drama” and “lives the Girl Scout values”.
Conclusion: Gendered differences exist in letters of recommendation for transplant surgery fellowship applicants. This research may provide insight into the inherent gender bias that is revealed in letters supporting candidates entering the field. This is the largest published study to identify differences in terms, length, and family references in a cohort of residents applying for a surgical fellowship.