J. S. Vazquez1,2, J. L. Clifford3, M. C. Bravo4, T. Orfeo4, M. McLawhorn2, L. T. Moffatt2, K. E. Brummel-Ziedins4, J. W. Shupp1,2 1MedStar Washington Hospital Center,The Burn Center, Department Of Surgery,Washington, DC, USA 2Firefighters’ Burn And Surgical Research Laboratory,Washington, DC, USA 3U.S Army Center For Environmental Health Research,Fort Detricj, MD, USA 4University Of Vermont,Department Of Biochemistry,Colchester, VT, USA
Introduction:
Mass casualty incidents could potentially create polytrauma injuries with extensive ionizing radiation (IR) exposure. Studies have demonstrated that radiation-induced coagulopathy (RIC) and associated hemorrhage occurring as part of the acute radiation syndrome is one of the principle causes of death in humans from radiation exposure. This phenomenon can occur at doses near the LD50, where RIC can result in bleeding, microvascular thrombosis, and multi-organ failure. In order to gain detailed insight into the effects of IR on biological systems we conducted a two-model approach: 1) radiation dose response and time course experiments in mice involving a skin transcriptome analysis and 2) exposure of whole human blood ex-vivo to IR.
Methods:
Groups of C57 black mice (n=5/cohort) were exposed to whole body X-ray at total doses of 0, 1, 3, 6, or 20Gy. Skin biopsies were obtained at serial time points post irradiation (Day 0, 4, 7, 14, 21, 28) and RNA isolated for microarray analysis. Ingenuity Pathways Analysis (IPA) software was used to identify gene networks with genes differentially expressed >2-fold between 20Gy and 0Gy groups at days 0, 4, and 7. Healthy human blood was exposed ex-vivo to IR at a dose of 5Gy and analyzed immediately post-exposure or at 40 min post-exposure by rotational thromboelastometry (ROTEM). Both groups were compared to non-irradiated blood as a control. Thrombin generation assays (TGA) using plasma isolated from exposed blood were performed.
Results:
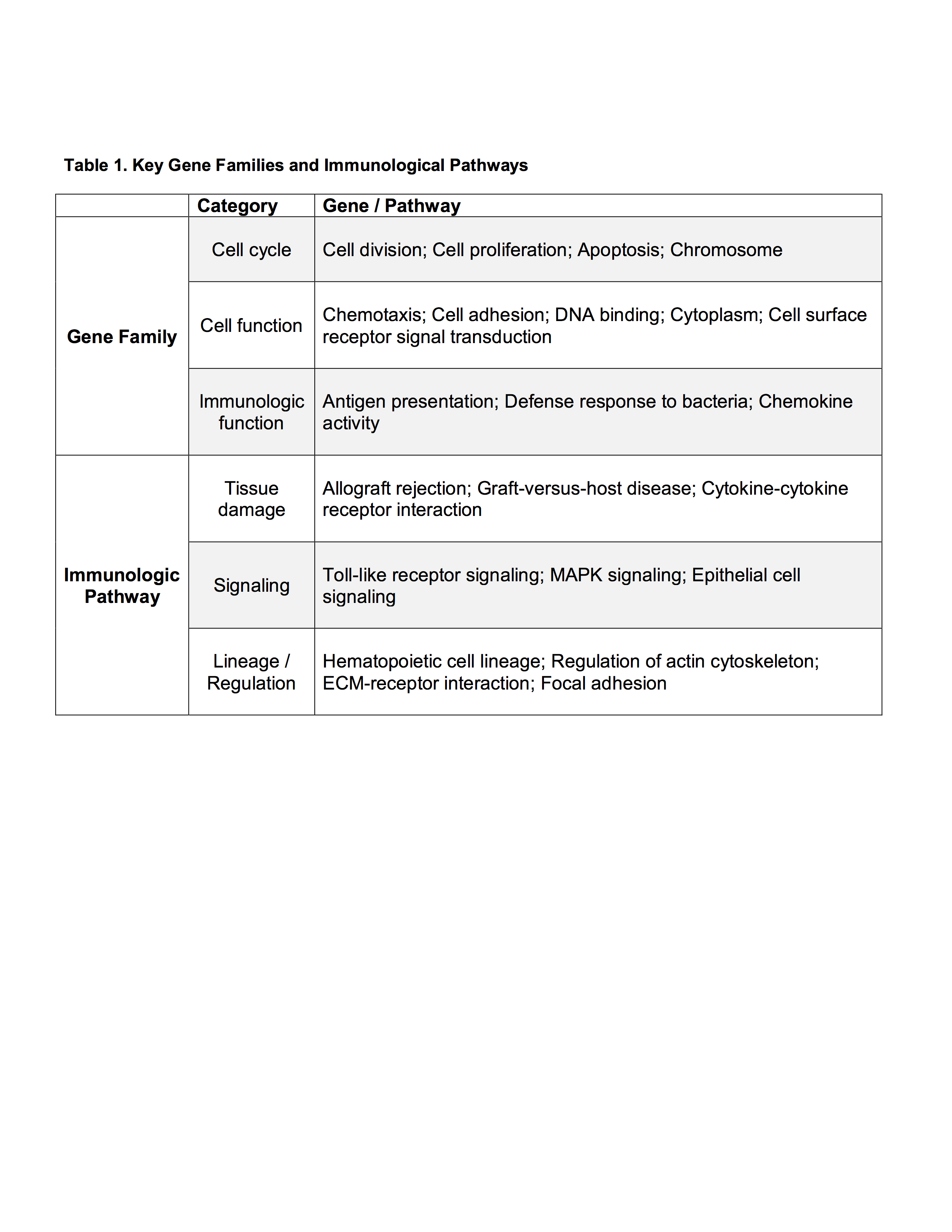
Sammon plots showed that gene expression in mice clustered along both time and dose parameters. We observed a clear separation of the mice receiving the highest dose of radiation (20Gy), and within this group a separation with time following radiation exposure. An initial comparison was made for genes exhibiting a 2-fold or greater difference in expression between 0 and 20Gy exposure, with a P value < 0.01. IPA software revealed a number of significantly altered gene functional networks, including the hematological system as well as networks related to dermatological disease and conditions, molecular transport, cell death and survival, lipid metabolism, and others. A particular gene of interest is ADTRP (androgen-dependent tissue factor pathway inhibitor (TFPI) regulating protein) which was downregulated in the fourth ranked gene network at Day 0. The TGA and ROTEM analyses demonstrated that the ex vivo human blood samples were more procoagulant post irradiation.
Conclusion:
The mouse model reveals distinct dose and time dependent differences in gene expression. ADTRP appears to be downregulated which would lead to a decreased expression and activity of the natural anticoagulant TFPI. Decreased TFPI may account for the procoagulant profile seen in our ex-vivo human blood exposed to IR. ADTRP may be a formidable candidate marker of radiation exposure and RIC and is deserving of further studies.