J. Robinson1,2, H. Huth4, G. P. Jackson2,3 1Vanderbilt University Medical Center,Department Of General Surgery,Nashville, TN, USA 2Vanderbilt University Medical Center,Department Of Biomedical Informatics,Nashville, TN, USA 3Vanderbilt University Medical Center,Department Of Pediatric Surgery,Nashville, TN, USA 4Vanderbilt University,Nashville, TENNESSEE, USA
Introduction: Government regulations, such as ‘meaningful use’, and consumer demand have driven widespread implementation and adoption of health information technologies. The emergence of electronic health records (EHRs), computerized order entry (CPOE), and patient portals has transformed the way health information is stored, used, and communicated to patients. The effect of such technologies on surgical practice has not been well studied. Our objective is to systematically review the available evidence regarding the impact of health information technology (HIT) on the care of surgical patients.
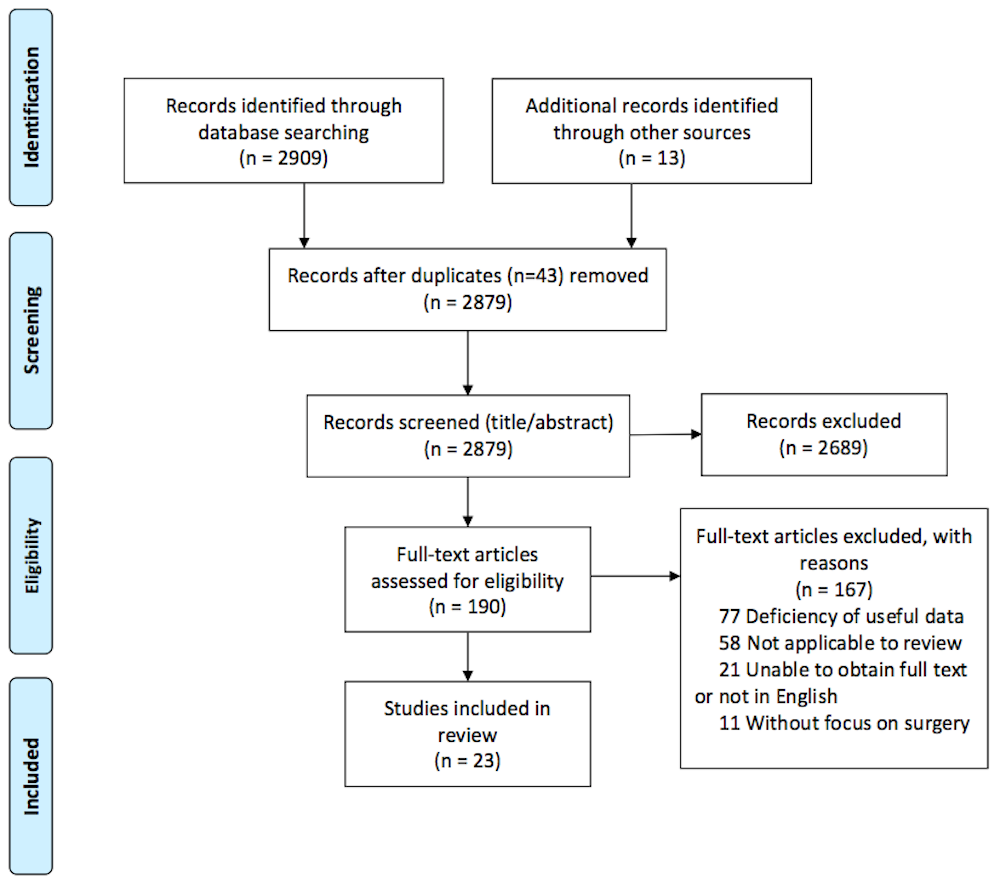
Methods: A systematic search of Medline, EMBASE, CINAHL, and Cochrane Library to identify data-driven, non-survey, studies on the effect of HIT, EHR, CPOE or patient portals on surgeons and their patients was performed. Experts in clinical informatics were also queried for known relevant articles to compile for review. Two authors independently reviewed abstracts to select relevant publications that met the inclusion criteria, followed by a full-text review of relevant articles, according to the PRISMA guidelines.
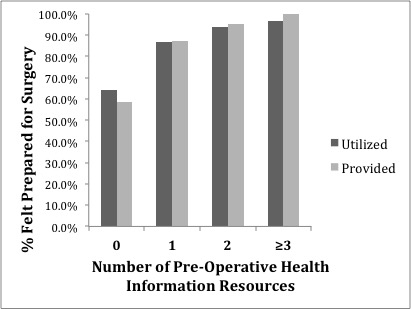
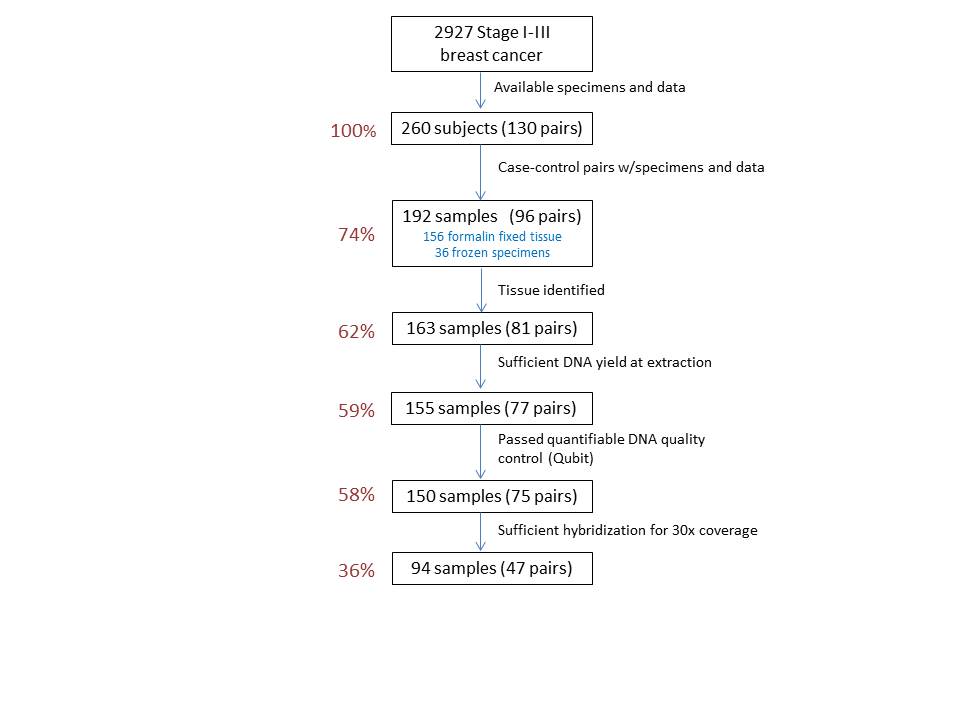
Results: A total of 2909 citations from 4 databases were identified, with 2879 publications remaining after duplicates were removed and the addition of expert-recommended articles. 190 articles were retrieved for full-text analysis, and 23 articles, including 21 observational studies and 2 RCTs, were found applicable. EHR and CPOE systems improved appropriate and timely antibiotic administration for surgical procedures in 6 observational studies. 5 observational studies indicated electronically generated operative notes have increased accuracy, completeness, and timely availability in the medical record compared to dictated notes. The Internet as an informative resource was inadequate for surgical procedures in 2 observational studies; however, a tailored web-based program decreased perioperative anxiety of patients in a single small-scale RCT. In observational studies, patient web portals showed high adoption and utilization, encompassing an increasing proportion of outpatient surgical encounters.
Conclusion: Overall, the quality of evidence on HIT in surgical practice found was moderate to low with only 2 RCTs identified. Currently available data suggest EHR, CPOE, and electronic notes are effective at improving the accuracy of drug administration and operative reports, but few other effects are known. While patient portals are in use, data is lacking on the quality or effect of portal encounters, and the Internet alone has not proven to be a reliable information source. With the increasing use of HIT in surgical patient care, further evidence-based research is required to optimize its utilization and efficacy.