H. A. Pitt1,2, A. J. Goldberg2, A. S. Pathak2, J. A. Shinefeld1, S. M. Hinkle1, S. O. Rogers2, V. J. DiSesa1,2, L. R. Kaiser1,2 1Temple University,Health System,Philadelpha, PA, USA 2Temple University,Department Of Surgery,Philadelpha, PA, USA
Introduction: Survival of surgical inpatients is a key quality metric. Patient, surgeon and system factors all contribute to inpatient mortality, and sophisticated risk adjustment is required to assess outcomes. When mortality of general surgical patients was determined to be high at a safety-net hospital (53% Medicaid/Medical Assistance), a comprehensive approach was undertaken to improve patient survival. The aim of this analysis is to demonstrate that risk-adjusted mortality can be improved at an essential hospital through implementation of numerous best practices.
Methods: General surgical service line mortality was measured in the University HealthSystem Consortium (UHC) database from January 2013 through March 2015. Ten best practices were sequentially undertaken to reduce observed (O) and/or increase expected (E) mortality. These quality efforts included a) recruitment of new surgeons, b) participation in ACS-NSQIP, c) hardwiring Surviving Sepsis elements, d) increasing the number of diagnostic codes submitted, e) standardizing documentation in Preoperative Anesthesia Testing, f) expanding Palliative Care consultations, g) implementing an aspiration prevention protocol, h) initiating 100% mortality review, i) adopting an Early Warning System to detect sepsis and j) enhancing patient selection and preparation for surgery. UHC mortality rank, O, E and O/E ratios as well as early deaths were compared with control charts for the 27-month analysis. Statistical significance was set at the p<0.05 level. Case Mix Index, a financial metric which correlates positively with patient severity and procedure complexity, was monitored over the same time period.
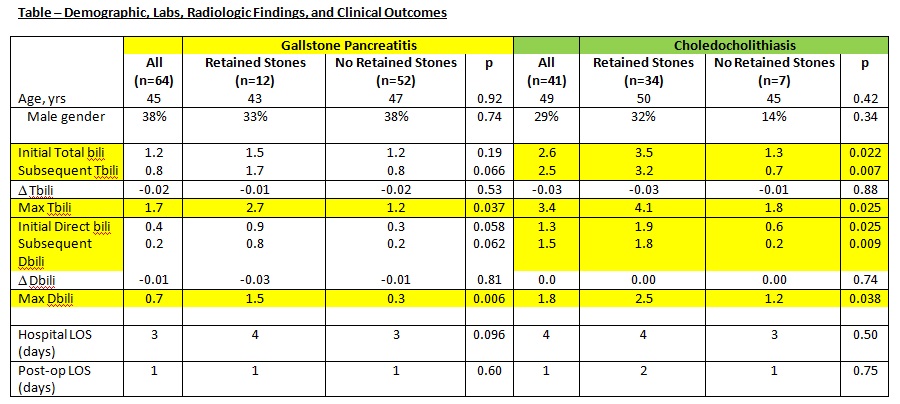
Results:UHC general surgery mortality rank improved from the bottom decile to the top quartile among 102 Academic Medical Centers. Mortality data by quarter (Q) are presented in the Table.
During this time, Case Mix Index increased from 2.48 in Q1 2013 to 2.91 in Q1 2015.
Conclusion:Risk-adjusted mortality and early deaths decreased significantly over 27 months in general surgery patients. During this time, patient and procedure complexity increased by 17 percent as measured by Case Mix Index. Systematic implementation of quality best practices assured surgical patient survival at a safety-net medical center.