E. A. Bailey1, G. C. Karakousis1, R. Hoffman1, M. Neuwirth1, R. R. Kelz1 1Hospital Of The University Of Pennsylvania,Department Of Surgery,Philadelphia, PA, USA
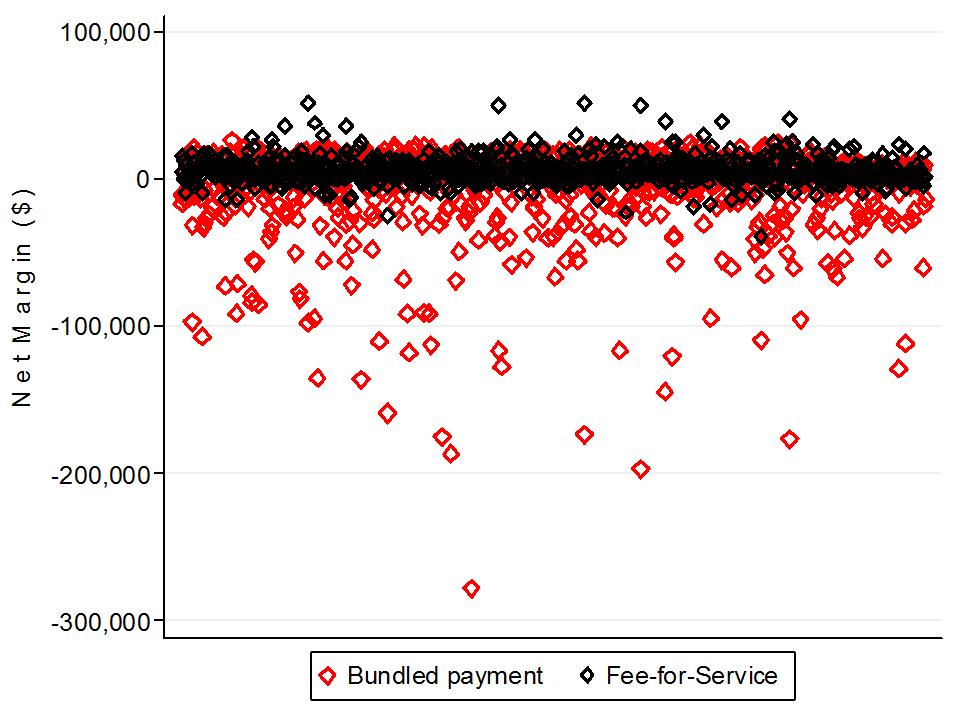
Introduction: As payment models move toward bundled reimbursement for an entire episode of care, including services provided after discharge, it is important to reduce excess utilization of costly inpatient care. The aim of this study was to compare inpatient length of stay (LOS) and cost differences for colorectal cancer surgery patients who did not experience complications and were discharged to home versus a post-acute care facility. We also sought to identify risk factors associated with discharge to a facility.
Methods: All patients who underwent surgical resection for colorectal cancer in New York and California in 2009-2010 and were discharged to home or to post-acute care (skilled nursing facility or inpatient rehab) were identified.. Patients were excluded if they had a surgical complication or a LOS greater than the 75th percentile for a given procedure. Median LOS and median cost per hospitalization were calculated. A multivariate logistic regression analysis was performed to assess preoperative risk factors associated with discharge to post-acute care.
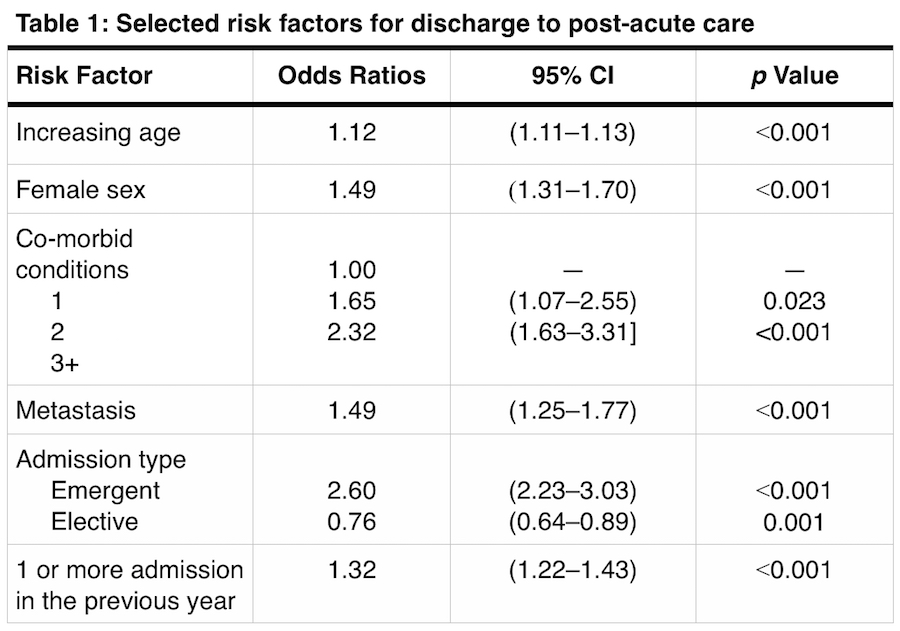
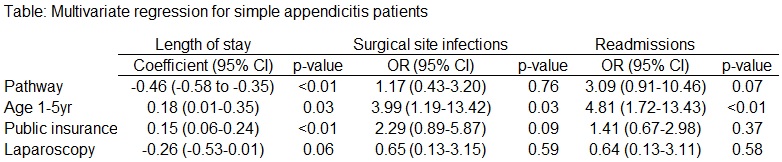
Results: Of the 35,807 patients initially identified, 11,946 (33.3%) were excluded for procedure-specific prolonged LOS or surgical complication. 23,861 patients were included in the study. Most patients were discharged to home (n=22,567, 94.6%) while 1,285 (5.4%) patients were discharged to a post-acute care facility. Patients discharged to home had a shorter median LOS (5 days [IQR 4,7]) than those discharged to a facility (7 days [IQR 6,9], p<0.001). Cost per hospitalization differed significantly between the two groups with a median of $16,882 (IQR $11,876, $24,146) per patient visit in the group discharged to home versus $20,705 (IQR $14,372, $28,208) in the group discharged to post-acute care (p<0.001). Factors associated with discharge to post-acute care by multivariate analysis included advanced age, female sex, race, 3 or more co-morbid conditions, presence of metastasis, emergent admission, at least 1 admission in the previous year, and being a Medicare patient (Table 1).
Conclusion: Even in the absence of a surgical complication, LOS following colorectal surgery was 2 days longer and $3,823 more costly for patients discharged to a post-acute care facility. Pre-operative factors such as age, sex, number of medical co-morbidities, and emergent nature of admission were significantly associated with a lower rate of being discharged to home. Early consultation with patient advocates and social services for discharge planning should be initiated for at risk patients to ensure a timely discharge and commencement of the true recovery process.