J. C. He2, L. A. Kreiner2, N. Sajankila1, D. L. Allen3, J. A. Claridge2 1Case Western Reserve University School Of Medicine,Cleveland, OH, USA 2MetroHealth Medical Center,Department Of Surgery,Cleveland, OH, USA 3Northern Ohio Trauma System,Cleveland, OH, USA
Introduction:
The optimal number of level I trauma centers (L1TCs) in a region has not been elucidated. To begin addressing this, we compared mortalities for patients injured in counties or regions with 1 L1TC to those with more than 1 L1TC.
Methods:
Recent state trauma registry data from 2010-2012 were analyzed. Trauma patients with age ≥15 from counties or regions with L1TC were included in this study. Region was defined as a L1TC containing county and its neighboring counties. Counties boarding more than one L1TC containing county were excluded from analysis. Two analyses were performed. For the county-level analysis, counties containing only 1 L1TC were compared to counties with more than 1 L1TC. For the regional analysis, regions covered by only 1 L1TC were compared to regions covered by greater than 1 L1TC. The following patient subgroups were included a priori for both analyses: Injury Severity Score (ISS) ≥ 15, age ≥ 65, and trauma mechanisms.
Results:
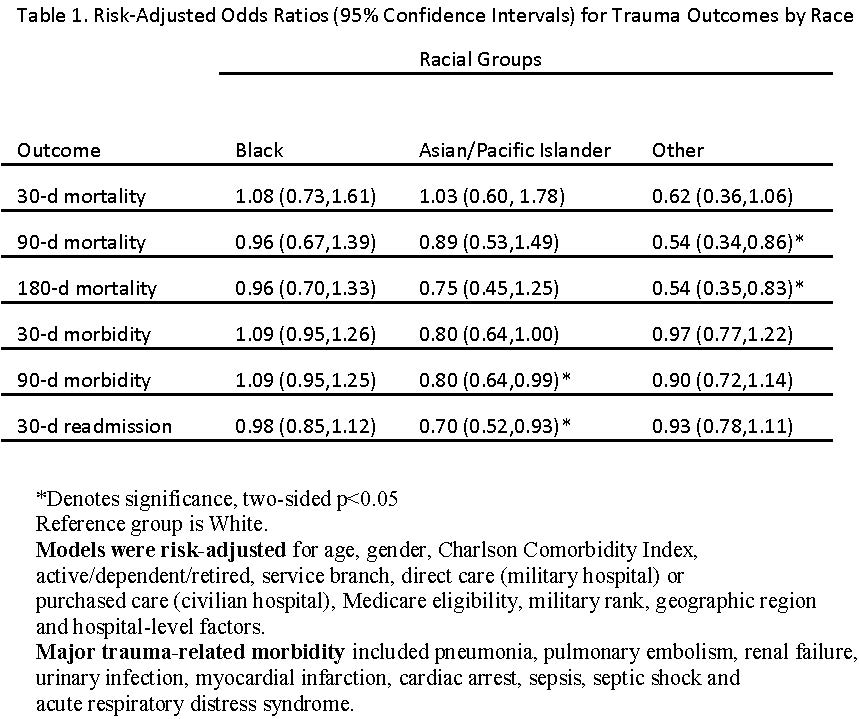
A total of 54,471 patients were analyzed. Their mean age was 59; 90% had blunt injuries. Their median ISS was 5, and the overall mortality was 4.8%. Both the county-level and regional analyses showed that patients in counties or regions with only 1 L1TC were older (60 vs. 57, p<0.001), but had similar ISS as compared to patients in counties or regions with more than 1 L1TC. Counties and regions with only one L1TC also had less total number of trauma centers (3.5 vs. 3.8 and 2.4 vs. 2.9, respectively; all p <0.001) Mortalities for the county-level and regional analyses for all patients and patient subgroups are compared in Table 1. Multivariable logistic regression adjusting for age, ISS and trauma mechanism demonstrated that having more than 1 L1TC in a region was an independent predictor for death (Odds Ratio=1.2; 95% CI: 1.1-1.3, p<0.001).
Conclusion:
Despite older patients and fewer total number of trauma centers, counties and regions with only one L1TC had lower mortality. This suggests that having multiple L1TCs in a county or region may not lead to increased patient survival.